What Are the Uses of Hyaluronic Acid in Bone Tissue?
Bone tissue defects caused by trauma, tumour, congenital malformation, infection and other pathological factors are one of the problems faced by clinical orthopaedics, and bone grafting is the main method to solve this problem [1]. Bone grafting is mainly divided into autologous bone grafting, allogeneic bone grafting or alloplastic bone grafting, but autologous bone grafting faces many problems, such as insufficient amount of autologous bone, easy to be infected and re-traumatise the patient, etc. Allogeneic bone grafting is expensive. Allogeneic bone grafting is expensive and has immune rejection. Tissue-engineered biomaterial bone as a substitute for bone repair materials can avoid the defects of biogenic repair materials [2].
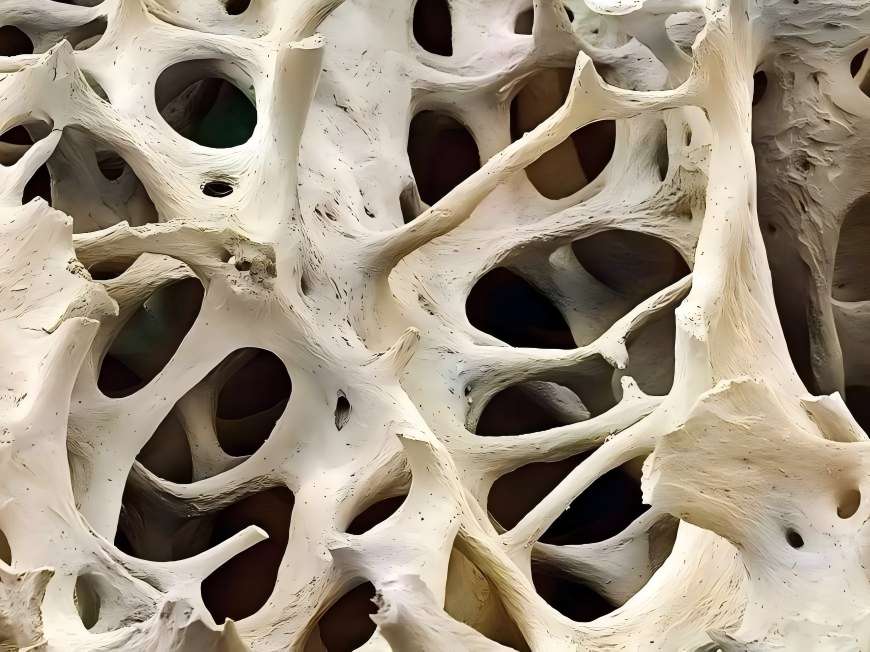
Ideal tissue scaffolds should have some properties: good biocompatibility; appropriate biodegradability and eventual disappearance; good cell-cell interface of the material to allow cell adhesion, promote cell growth, and retain cell differentiation; three-dimensional porous structure and good porosity to allow cell infiltration and vascularisation; and a certain degree of mechanical strength, which is easy to fabricate [3]. Hyaluronic acid is a new hot spot in the research of bone biomaterials. Hyaluronic acid has a high degree of viscoelasticity, plasticity, excellent water absorption, permeability and good bioabsorbability, and is non-immuno-antigenic. Modified hyaluronic acid not only maintains the original superior properties, but also improves its properties and makes it more adaptable to the human environment [4]. Therefore, hyaluronic acid is now the hot spot of bioengineering bone tissue materials.

1 Application of hyaluronic acid in osteoarthritis treatment
Osteoarthritis is one of the most common knee injuries and joint diseases, and injection of hyaluronic acid (sodium vitrate) has become a common treatment for osteoarthritis. According to the literature, Manicourt et al[5] reported that the content of hyaluronic acid increased when the physiological stress in the joint increased, which suggests that hyaluronic acid, as an important component of proteoglycan polymers, may have a buffering effect on stress. Hyaluronic acid in synovial fluid has a large amount of negative charge when combined with proteins, and it has strong water absorption and high viscosity. Proteoglycan polymers increase the lubricity and viscoelasticity of the synovial fluid and provide a high affinity between the lubricant and the articular cartilage. Hyaluronic acid and proteoglycans adhere tightly to the joint surfaces and act as lubricants, thus reducing the resistance to joint movement and protecting the articular cartilage from excessive mechanical wear.
Kawasaki et al.[6] reported that hyaluronic acid increased the synthesis of chondroitin sulphate by chondrocytes cultured in collagen gels, and Stove et al.[7] found that hyaluronic acid decreased the production of proteoglycans by chondrocytes in osteoarthritic patients, but hyaluronic acid inhibited the reduction of proteoglycans induced by IL-1, and Kikuchi et al.[8] reported that exogenous hyaluronic acid increased the production of chondroitin in seaweed beads. Kikuchi et al.[8] reported that exogenous hyaluronic acid caused the movement of newly synthesised proteoglycans from pericellular to distal matrix of chondrocytes in algal bead medium and cartilage tissues, suggesting that hyaluronic acid may have an effect on the distribution and movement of proteoglycans, and may have a protective effect on the cartilaginous extracellular matrix. In addition, hyaluronic acid is a scavenger of free radical cellular debris, embedding itself in the polymer meshwork formed by hyaluronic acid and metabolising it rapidly within the joint, thus contributing to the elimination of cellular debris and assisting in the elimination of cartilage cellular metabolites.
2 The combination of hyaluronic acid and biofactors in the repair of cartilage and bone defects
2.1 Promoting chondrocyte proliferation
After cartilage damage, its own repair ability is limited, and the use of chondrocyte transplantation is the current hot spot. Studies have shown that insulin-like growth factor-1 plays an important role in cartilage repair. Hyaluronic acid is one of the main components of cartilage matrix. According to the literature, insulin-like growth factor-1 is the first growth factor that has been identified to have a regulatory effect on articular chondrocytes. However, it has a short half-life, is easily degraded, and is susceptible to interference by internal factors, thus limiting its effects [9-10].
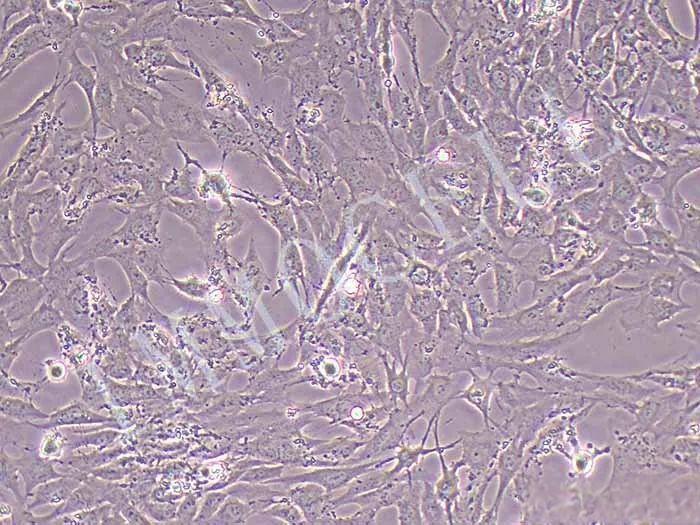
Hyaluronic acid is negatively charged, has strong hydrophilicity and high adhesion, and has strong affinity with chondrocytes. In addition, hyaluronic acid has the function of chondroinduction, which can provide nutrition for articular chondrocytes, participate in the synthesis of proteoglycan polymers, act as a building block on the surface of chondrocytes through glycoproteoglycans, and promote the proliferation of superficial joints, maintain the thickness of uncalcified cartilage, and promote the repair of articular cartilage with degenerative changes to a certain extent [11-12]. It has been reported in the literature that the combination of hyaluronic acid and insulin-like growth factor-1 in the in vitro culture of human articular chondrocytes can help to maintain the stability of the phenotype of hyaluronic acid chondrocytes and promote the proliferation of the cells, thus providing a new method to obtain high-density autologous chondrocytes in vitro that have normal functions, and also providing experimental bases for the study of autologous chondrocyte transplantation or cartilage tissue engineering [13].
2.2 Composite allograft
The commonly used material for the repair of segmental bone defects is allogeneic freeze-dried bone, but due to the weak induced activity of allogeneic freeze-dried bone and its poor osteogenic ability, it only serves as a scaffold for osteoconduction in the process of repair. The development of modern molecular biology technology has led to a deeper understanding of the osteogenic and osteoinductive activities of bone growth factors, and bone grafts containing bone growth factors combined with suitable carriers have become a new trend in the treatment of bone defects. It has been reported in the literature that implantation of basic fibroblast growth factor fused with hyaluronic acid gel and composite freeze-dried bone into the bone defect area has a good effect on repairing bone defects [14-15]. BFGF can stimulate the proliferation of mesenchymal cells, chondrocytes and osteoblasts, and induce the differentiation of mesenchymal cells to bone and chondrocytes; stimulate the proliferation of vascular endothelial cells, and promote the formation of neovascularisation [16].
Based on the above biological properties of basic fibroblast growth factor, it was compounded with hyaluronic acid and freeze-dried bone to promote the growth of osteoblasts by taking advantage of their respective strengths. The histological sections of this experiment showed that: in the early stage, a large number of mesenchymal cells could be seen in the bone defect area of the complex containing basic fibroblasts, hyaluronic acid and lyophilized bone, bridging the bone fracture in the form of cords, and showing a tendency of differentiation to osteoblasts and chondroblasts, with the appearance of new bone and cartilage islands; in the mid-stage, the neovascularisation grew into the area, and the cartilage tissues matured in the process of ossification, with the islands fused together into a piece to form a braided bone. The amount of new bone and cartilage in the hyaluronic acid and lyophilised bone group was significantly lower than that in the basic fibroblast, hyaluronic acid and lyophilised bone complex group, and the distribution was uneven [17].
It has been reported in the literature that the role of basic fibroblast growth factor is to stimulate the proliferation of mesenchymal cells at the beginning of bone repair, and the latter form cartilage scabs and act as a growth factor and other osteoinductive factors to stimulate osteoblasts to differentiate into osteoblasts or chondrocytes, initiating the process of defect repair. With the growth of neovascularisation, the blood supply to the graft is re-established, promoting endochondral ossification, accelerating graft replacement and maturation of new bone, and shortening the healing time. As a matrix, hyaluronic acid can provide nutrients and three-dimensional space for cell growth, which is conducive to the repair of bone tissue [18].
3 Application of modified hyaluronic acid complexes in biological bone tissue
Hyaluronic acid is easily degraded and its degradation time is closely related to its molecular weight. Therefore, in order to prolong the degradation time of hyaluronic acid molecules in the organism, it is necessary to prepare a derivative with a much higher molecular weight than that of natural sodium hyaluronate molecules, i.e., cross-linked sodium hyaluronate derivatives, through chemical modification. The principle of preparation of cross-linked sodium hyaluronate is to use one or more combinations of chemical cross-linking agents, using the cross-linking agent (oxidation, reduction, esterification, aldolisation, etc.) to make the hyaluronic acid molecules undergo a chemical reaction, so that the hyaluronic acid molecules or hyaluronic acid and the cross-linking agent cross-linking together [19].
The cross-linking reaction lengthens the hyaluronic acid molecules, increases or decreases their solubility properties, and improves their mechanical strength or resistance to degradation by the body. Therefore, various chemical modifications of hyaluronic acid have been carried out and applied to the study of bone tissue engineering. Martinez-Sanz et al. used aminopropanetriol as a cross-linking agent to form perylene-HA matrix by amidation, and this hyaluronic acid derivative complexed with bone-forming protein-2 was proved to be non-cytotoxic and histocompatible in in vitro tests. When the compound was injected into the cranial surface of rats, histological examination showed that there was new bone formation on the cranial surface after 8 weeks, and the expression of osteocalcin and bone marrow angiogenesis was also high, which means that perylenic-hyaluronic acid can act as a carrier of osteoblast-2 and can promote bone expansion. This finding has been confirmed by subsequent studies [18-19].
Bae et al.[20] observed the effects of photocured hyaluronic acid in combination with simvastatin on bone regeneration. The results showed that the viscoelasticity of the 2-aminoethyl methacrylate-hyaluronic acid matrix was significantly improved compared with that of hyaluronic acid, and that it could regulate the stable and slow release of simvastatin, which promoted the increase of MC3T3-E1 cell proliferation. MC3T3-E1 cells proliferated and differentiated, thus inducing new bone formation, i.e., photo-hyaluronic acid combined with simvastatin could be a good scaffold for tissue-engineered bone.

Lisignoli et al.[21] investigated the osteogenesis of hyaluronic acid derived from its esterification, benzyl ester of hyaluronic acid, in combination with bone marrow stromal cells in a murine model of large bone defects, where the cells were treated with alkaline fibroblast growth factor supplemented or not with supplemented mineralisation medium, and the results showed a significant increase in the viscosity of the matrix. Cells were cultured in mineralisation medium with or without alkaline fibroblast growth factor supplementation, and defect healing was evaluated after 40, 60, 80 and 200 d. In vivo studies have demonstrated that benzyl hyaluronate is a suitable vehicle for bone defect repair and significantly accelerates bone mineralisation when combined with bone marrow stromal cells and alkaline fibroblast growth factor.4 Hyaluronic acid complexes with growth factors are also suitable for bone repair.
4 Hyaluronic acid complexes combined with growth factors in bone tissues
Hyaluronic acid is a good carrier of growth factors in bone repair, but its main drawback as a scaffold is its low cell adhesion properties, whereas integrins are a major family of cell surface receptors that mediate the adhesion of cells to the extracellular matrix.23 Kisie et al. [24] covalently bonded hyaluronic acid with specific ligands on integrins to form a hyaluronic acid-integrin matrix and investigated the effects of hyaluronic acid-integrin complexes in large bone defects in a murine model.
Compared with the control group, the hyaluronic acid-integrin hydrogel showed a significant increase in cell adhesion and bone growth factor delivery, which further enhanced the osteogenic potential of recombinant human osteoblast-2. Therefore, the hyaluronic acid-integrin matrix can be used as a growth factor delivery vehicle, and has a potential value for clinical application. The study of hyaluronic acid complex is the hot spot of biomaterials research nowadays, this kind of complex combines the advantages of its own material and makes up for its own shortcomings, which has the incomparable advantages of other materials, but there is no in-depth study on the histocompatibility, inflammation and degradability of this kind of composite, which may be the hot spot of future research.
5 Problems and prospects
Hyaluronic acid is a biodegradable biomaterial with good biocompatibility, and its hydrophilicity plays an important role in cell adsorption, growth and differentiation. It can be used as a temporary skeleton to support and stimulate the growth of new bone tissues, and then it will be gradually degraded to be replaced by new bone tissues after completing the mechanical support function for a certain period of time. A large number of experimental studies have proved that hydrogels based on hyaluronic acid and compounded with insulin-like factor, growth factor and BMP-2 can provide a growth environment for chondrocytes, osteoblasts and myeloid cells, and their three-dimensional structure, good water solubility, no immune reaction and good degradability are the advantages of hyaluronic acid [28-29], but there are still a lot of difficulties that need to be overcome if they are applied in clinical practice. Hyaluronic acid has been discovered for more than 80 years. Hyaluronic acid has been discovered for more than 80 years, and has been used in ophthalmology, joint surgery and other research fields [30-33], and it is a new development to use it as the basis of biomaterials for biological tissues. In recent years, there have been many experimental researches on biomaterials using hyaluronic acid as scaffolds, and it is hoped that it can be really used in the clinic in the near future.
Reference
[1]Silber JS,Anderson DG,Daffner SD,et al.Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion[J]. Spine ,2003 ,28 : 134 - 139.
[2]Salgado AJ ,Coutinho OP ,Reis RL. Bone tissue engineering :state of the art and future trends[J].Macromol Biosci,2004,4 : 743-765.
[3]O'Brien FJ.Biomaterials & scaffolds for tissue engineering[J]. Materials Today,2011,14(3) : 88-95.
[4]Bae MS,Yang DH,Lee JB,et al.Photo-cured hyaluronic acid- based hydrogels containing simvastatin as a bone tissue regeneration scaffold[J]. Biomaterials,2011,32 ( 32 ) : 8161 - 8171.
[5]Manicourt DH, Pita JC, Thonar EJ. Proteoglycans nondissciatively extracted from different zones of canine normal cartilage[J].Connect Tissue Res,1991,26 :231-246.
[6]Kawasaki K,Ochi M,Uchio Y. Hyaluronic acid enhances proliferation and chondrointinsulfate synthesis in cultured chondrocytes embedded in collagen gel [J].Cell Physiol ,1997, 179 : 142-148.
[7]Stove J,Gerlach C,Huch K.Effects of hyaluronan proteoglycna content of osteoarthritic chondrocytes in vitro[J].J Orthop Res, 2004,20(3) : 551-555.
[8]Kikuchi T ,Yamada H ,Fujikawa K. Effects of high molecular weight hyaluronan on the distribution and movement of proteoglycan around chondrocytes cultured in alginate beads[J]. Osteoarthritis Cartilage,2001,9(4) : 351-356.
[9]Huang Jianrong,Liu Shangli,Song Weidong,et al.Insulin-like growth factor type 1 and hyaluronic acid on human embryo articular cartilage cells phenotypic effects[J]. Journal of Sun Yat-sen University : Medical Sciences,2002,23 (6) :419-422.
[10]Baldini A,Zaffe D ,Nicolini G. Bone-defects healing by high- molecular hyaluronic acid:preliminary results [J]. Ann Stomatol : Roma,2010,1 ( 1) : 2-7.
[11]Ossipov DA, Piskounova S, Varghese OP, et al. Functionalization of hyaluronic acid with c hemoselective groups via a disulfide-based protection strategy for in situ formation of mechanically stable hydrogels[J].Biomacromolecules,2010,11 (9) : 2247-2254.
[12]Martinez-Sanz E,Ossipov DA,Hilborn J,et al.Bone reservoir : Injectable hyaluronic acid hydrogel for minimal invasive bone augmentation[J].Control Release,2011,152(2) : 232-240.
[13]Varghese OP,Sun W,Hilborn J,et al In situ cross-linkable high molecular weight hyaluronan-bisphosphonate conjugate for localized delivery and cell-specific targeting:a hydrogel linked prodrug approach[J].Am Chem Soc,2009,131 : 8781-8783.
[14]Li Shouhong ,Pang Guangming ,Chen Jiangang ,et al.Sodium hyaluronate gel composite TGF-beta 1 to repair rabbit mandibular defect of experimental research[J]. Journal of Clinical Oral Medicine,2008,24(3) : 157-159.
[15]Kisiel M,Martinomm,Ventura M,et al. Improving the osteogenic potential of BMP-2 with hyaluronic acid hydrogel modified with integrin-specific fibronectin fragment [J]. Biomaterials,2013,34(3) :704-712.
[16]Zhang Junhui ,Chen Yongqiang,Tang Tingting ,et al.Hyaluronic acid compound BMP-2 transfection between bone marrow mesenchymal stem cells to repair rabbit radial backbone bone injury[J].Chinese Journal of Orthopaedics ,2005,25( 10) : 608-612.
[17]Jin R,Teixeira LS,Dijkstra PJ,et al .Enzymatically crosslinked injectable hydrogels based on biomimetic dextran-hyaluronic acid conjugated for cartilage tissue engineering[J]. Biomaterials, 2010,31 ( 11) : 3103-3113.
[18]Ossipov DA,Piskounova S ,Varghese OP,et al.Functionalization of hyaluronic acid with chemoselective groups via a disulfide-based protection strategy for in situ formation of mechanically stable hydrogels[J].Biomacromolecules,2010,11 (9) : 2247-2254.
[19]Martinez-Sanz E,Ossipov DA,Hilborn J,et al.Bone reservoir : injectable hyaluronic acid hydrogel for minimal invasive bone augmentation[J].J Control Release,2011,152(2) : 232-240.
[20]Martinez-Sanz E,Varghese OP ,Kisiel M ,et al.Improving the osteogenic potential of BMP -2 with hyaluronic acid hydrogel modified with integrin-specific fibronectin fragment[J]. Biomaterials,2013,34(3) :704-712.
[21]Bae MS,Yang DH,Lee JB,et al.Photo-cured hyaluronic acid- based hydrogels containing simvastatin as a bone tissue regeneration scaffold[J]. Biomaterials,2011,32 ( 32 ) : 8161 - 8171.
[22]Calderon L,Colline E,Velasco-Bayon D,et al. Type Ⅱ collagen-hyaluronan hydrogel-a step towards a scaffold for intervertebral disc tissue engineering[J].EUR Cell Mater,2010, 20 : 134-148.
[23]Lisignoli G ,Fini M ,Giavaresi G ,et al. Osteogenesis of large segmental radius defects enhanced by basic fibroblast growth factor activated bone marrow stromal cells grown onnon-woven hyaluronic acid-based polymer scaffold[J].Biomaterials,2002, 23 (4) : 1043-1051.
[24]Kisiel M,Martinomm,Ventura M,et al. Improving the osteogenic potential of BMP -2 with hyaluronic acid hydrogel modified with integrin-specific fibronectin fragment [J]. Biomaterials,2013,34(3) :704-712.
[25]Bae MS,Yang DH,Lee JB,et al.Photo-cured hyaluronic acid- based hydrogels containing simvastatin as a bone tissue regeneration scaffold[J]. Biomaterials,2011,32 ( 32 ) : 8161 - 8171.
[26]Guo N,Woeller CF,Feldon SE,et al.Peroxisome proliferator- activated receptor gamma ligands inhibit transforming growth factor-beta-induced ,hyaluronan-dependent ,T cell adhesion to orbital fibroblasts[J].J Biol Chem,2011,286 (21 ) : 18856 - 18867.
[27]Liu LS,Thompson AY,Heidaran MA,et al.An osteoconductive collagen / hyaluronate matrix for bone regeneration [J]. Biomaterials,1999,20( 12) : 1097-1108.
[28]Liu XW ,Hu J ,Man C ,et al. Insulin-like growth factor -1 suspended in hyaluronan improves cartilage and subchondral cancellous bone repair in osteoarthritis of temporomandibular joint [J].Oral Maxillofac Surg,2011,40(2) : 184-190.
[29]Docherty-Skogh AC,Bergman K,Waern MJ,et al. Bone morphogenetic protein-2 delivered by hyaluronan-based hydrogel induces massive bone formation and healing of cranial defects in minipigs[J].Plast Reconstr Surg,2010,125 (5) : 1383-1392.
[30]Hintze V,Moeller S ,Schnabelrauch M ,et al.Modifications of hyaluronan influence the interaction with human bone morphogenetic protein-4 ( hBMP-4) [J].Biomacromolecules, 2009,10( 12) : 3290-3297.
[31]Hannan FM,Athanasou NA,Teh J,et al. Oncogenic hypophosphataemic osteomalacia:biomarker roles of fibroblast growth factor 23 ,1,25 -dihydroxyvitamin D3 and lymphatic vessel endothelial hyaluronan receptor 1[J].Eur J Endocrinol, 2008,158 (2) : 265-271.
[32]Yang Fengquan,Sun Qingyan.Triple therapy for knee osteoarthritis[J].China Modern Medicine,2013,20 (25 ) : 39-40.
[33]Zhou Yanhong.Observation of the influence of sodium hyaluronate on the microcirculation and adhesion state of patients with uterus cavity operation during the perioperative period[J].China Modern Medicine,2014,21 (33) :46-48.


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese







