Study on the Clinical Uses of Hyaluronic Acid
Hyaluronic acid (HA) is also known as vitreous acid. It was first isolated in 1934 by Meyer and Palmer from the vitreous humor of the bovine eye[1] . Hyaluronic acid is also found in a wide range of tissues in the human body, including the vitreous humor of the human eye, umbilical cord and skin (Table 1), and is a component of the extracellular matrix [2]. Hyaluronic acid, chemically known as (1,4)-O-β-D glucuronide-(1,3)-2-acetamido-2-deoxy-β-D glucose, is a high molecular weight straight-chain glycan, a polymer formed by repeated alternation of alternating N-acetylglucosamine (GlcNAc) and glucuronide (GlcA) disaccharide units [3], with a wide range of molecular weights, and a formula ( C14H20NO11Na). C14H20NO11Na)n, the molecular weight of the disaccharide unit is 401.3 (Figure 1).
Due to the hydrogen bonding between the straight-chain L-monosaccharides, hyaluronic acid molecules are spatially rigid helical columns with a radius of 200 nm. Hyaluronic acid is strongly hydrophilic, and in aqueous solution, hyaluronic acid is about 1,000 times more hydrophilic than its own weight. In addition to hydrophilicity, hyaluronic acid solution has unique hydrodynamic properties, and its aqueous solution is a non-Newtonian fluid, therefore, it has good viscoelasticity and strain [4]. Currently, hyaluronic acid is widely used in biomaterials, drug-targeting agents, aesthetics, and the prevention of adhesions after abdominal surgery [5].
1 Applications of hyaluronic acid
1.1 Ophthalmic diseases
As an acidic mucopolysaccharide, hyaluronic acid is widely distributed in the intercellular matrix of various tissues of the human body, and has important physiological functions such as maintaining the stability of cellular osmotic pressure, and enabling the adhesion of adjacent cells [6]. In addition, hyaluronic acid can regulate cell adhesion and motility, regulate cell differentiation and proliferation, and maintain normal biomechanical properties of tissues[7] . Hyaluronic acid is widely used in ophthalmic surgery, mainly due to its viscous, pseudoplastic, elastic, adhesive and coating properties, which make it a viscoelastic liner, intra-tissue detachment, viscous obstruction, viscous haemostasis, viscoelastic cushioning, and elastic fixation [8].
Dry eye disease is a common ophthalmic syndrome, which is mainly caused by the dysfunction of ocular gland cells, including various types of conjunctivitis. Hyaluronic acid is rich in hydrophilic groups, which can bind with water molecules and act as a hydrophilic and lubricating agent, and thus can alleviate dry eye symptoms to a certain extent. According to the ‘Expert Consensus on Clinical Diagnosis and Treatment of Dry Eye (2013)’[9] , ‘The aim of dry eye treatment is to alleviate eye symptoms in patients with mild dry eye, and to protect visual function in patients with severe dry eye’. Sodium hyaluronate eye drops can flush and dilute inflammatory mediators on the ocular surface, reduce tear osmolarity, promote healing of the ocular surface epithelium, and promote the secretion and deposition of fibronectin on the ocular surface, which plays an important role in healing ocular surface epithelial injury. In a study of 106 patients with dry eye disease, Yu Huiling [10] found that 0.3% sodium hyaluronate eye drops alone were effective in 81.8% of cases of dry eye disease, while the combination of sodium hyaluronate eye drops and pranoprofen eye drops was effective in 92.3% of cases.

1.2 Medical cosmetology
Hyaluronic acid is often used as a moisturising ingredient in cosmetics, including hyaluronic acid moisturising and water-locking creams and moisturising and hydrating masks. 50% of hyaluronic acid exists in the human body. 50% of hyaluronic acid in the human body exists in the dermis of the skin, providing the spatial structure for the distribution of collagen fibres and elastin. Together they form the scaffolding of the skin, maintaining the stability of the skin tissue and preserving its elasticity. If one of them is absent, skin aging and wrinkle formation can be accelerated[11] .
Hyaluronic acid, as one of the components of human connective tissue and synovial fluid, is one of the most widely used dermal fillers in the world due to its high biocompatibility and is commonly used in the treatment of periocular wrinkles, crow's feet, and head lines [12-14]. Xue Zihan et al. injected 0.2 ml of hyaluronic acid into the facial ligaments of 23 patients with mild-to-moderate facial laxity, and there were no redness, swelling, pain, bruising, or allergic reactions in the 23 patients, and there were no adverse reactions, such as hard nodules, displacement of filler, vascular embolism, or skin necrosis. After the injection, all of them showed different degrees of improvement in the laxity of the eye corners and subzygomatic area, as well as enhancement of the forehead lines, elevation of the corners of the mouth, better definition of the mandibular margin, and firmer facial texture.
Follow-up showed that the effects of the injections lasted for about 3-6 months, and re-injections were required after half a year to maintain the effects[15]. Hyaluronic acid regulates collagen synthesis, reduces the production of inflammatory mediators, inhibits capillary exudation and fibrinogen deposition, and inhibits fibroblasts from synthesising collagen fibres, thus inhibiting the formation of surgical scars.16-18 Patel used a needle-free injection of cross-linked hyaluronic acid in two patients with acne scars, and then repeated the administration of hyaluronic acid once at an interval of 4 weeks, which was effective in reducing the degree of scarring without any adverse effect on patients. It can effectively reduce the degree of scarring without adverse effects [19].

1.3 Osteoarthropathy
Hyaluronic acid is an important component of synovial fluid and acts as a lubricant to protect the ends of bones [20]. When initially synthesised, hyaluronic acid consists mainly of high molecular weight hyaluronic acid polymers between 2×105 and 2×106 Da [21]. In osteoarthritis and rheumatoid arthritis, the molecular weight of hyaluronic acid becomes smaller and the synovial fluid viscosity decreases, resulting in a decrease in the viscoelasticity of hyaluronic acid, which leads to an increase in the wear and tear of joint surfaces [20]. Intra-articular injection of high molecular weight hyaluronic acid can effectively relieve the pain of patients with osteoarthritis and rheumatoid arthritis and play a certain therapeutic role[22] . In addition to its lubricating effect, hyaluronic acid can reduce the phagocytosis of macrophages and improve the inflammatory response[23].
Yuan Shuyan et al. injected 2.5 ml of sodium hyaluronate into the joint cavity of 35 patients with knee osteoarthritis and found that the patients' pain decreased and the level of IL-6β in the synovial fluid of the joints decreased after the administration of sodium hyaluronate.24 Seung found that cross-linked hyaluronic acid gel scaffolds were easy to be mixed with human dental pulp stem cells and mimetic peptides, and the mixture was easy to be injected. After injection into mice, cross-linked hyaluronic acid rapidly formed a hydrogel scaffold at the injection site and remained safely and without irritation for more than 8 weeks. Dental pulp stem cells can survive for at least 8 weeks in the hydrogel, and the mimetic peptide can induce the differentiation of dental pulp stem cells to osteoblasts, and the cross-linked hyaluronic acid gel scaffolds can be used as biomaterials for bone tissue engineering [25].

1.4 Prevention of postoperative adhesions
Hyaluronic acid is used to prevent postoperative adhesions, which can effectively reduce the incidence and severity of adhesions [26]. The mechanism of hyaluronic acid in preventing postoperative adhesions is as follows: (1) hyaluronic acid gel has a polymer fibre mesh structure, coated on the surface of the tissue, which can play the role of barrier, and form a short-lived protective barrier during peritoneal repair; (2) inhibit postoperative hemorrhage and oozing, reduce the number of blood clots that can form the structure of the permanent adhesions, and avoid the fibrin deposits in the contact surface of the tissue; (3) hyaluronic acid inhibits the migration and phagocytosis of neutrophil granulocytes, and reduces inflammation and inflammatory processes. (iii) Hyaluronic acid inhibits the migration and phagocytosis of neutrophil leukocytes and reduces inflammation [27]; (iv) Hyaluronic acid interacts with high affinity hyaluronic acid receptor proteins on the membrane surface of mesenchymal stromal cells and fibroblasts and improves the migration and chemotaxis ability of these cells, which promotes the in vivo repair process; (v) Hyaluronic acid gels are covered on the surface of the traumatised plasma membrane, and they are not degraded or metabolised for a certain period of time, so that the early wound repair can be carried out in a sustained and effective manner until a continuous wound is formed in the contact surface. ⑤ Hyaluronic acid gel covers the plasma membrane surface of the wound, and is not degraded and metabolised for a certain period of time, so that early tissue repair can be carried out continuously and effectively, until a continuous mesothelial cell layer is formed on the wound surface to complete tissue repair.
Cai Tongkai et al.[28] used a bilateral injury model of rat cecum and abdominal wall to determine the degree of abdominal adhesion by Nair adhesion 5-grade classification, and found that 30 d after surgery, the abdominal adhesion of SD rats in sodium hyaluronate gel group was significantly lower than that of the model group, and the limiting load and stiffness ratios of the sodium hyaluronate gel group were not statistically different from that of the sham-operated group and the model group. Medical sodium hyaluronate gel can effectively reduce the degree of adhesion and does not affect the recovery of trauma. Zhang et al. studied the efficacy of medical sodium hyaluronate and oxidised regenerated cellulose in the prevention of peritoneal adhesions in rats using a model of two uterine injuries, and found that both medical sodium hyaluronate and oxidised regenerated cellulose were effective in decreasing the degree of adhesion damage [27]. Solid membranes are difficult to fix accurately at the site of trauma and need to be removed surgically after tissue healing [29]. The liquid form of hyaluronic acid is not only easy to handle and cover the wound site, but also remains in the body for a period of time consistent with the wound healing cycle.
1.5 Drug carriers
In recent years, hyaluronic acid has been used as a drug carrier, reacting with other drugs to form compounds that exert slow-release and targeted effects so that the bound drug can be released in a timed or targeted manner[30-32] . As a nanomaterial, hyaluronic acid can be used to form targeted formulations with antineoplastic drugs for the treatment of pelvic tumours.Lee found that hyaluronic acid nanoparticles were readily endocytosed by colon cancer HCT116 cells from CD44 receptor-positive patients[33] , and nanocomplexes formed by conjugation of hyaluronic acid and paclitaxel showed enhanced cytotoxicity against HCT116 cells in vitro.34 Bajaj used hyaluronic acid with paclitaxel to form nanocomplexes with the same drug. Bajaj extended the retention time of paclitaxel in nude mice by encapsulating paclitaxel in hyaluronic acid colloid and effectively reduced the growth and metastasis of SKOV-3 tumour in human ovarian cancer[35] .
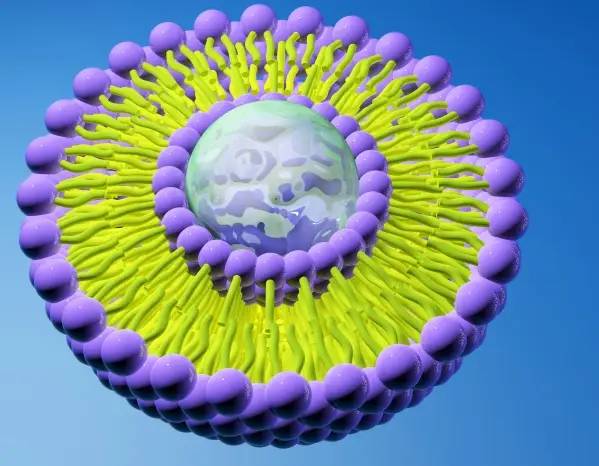
Xiao et al. used a lipid carrier with hyaluronic acid-octadecylamine structure to load paclitaxel, and the loading rate was increased to 72%. In nude mice, the distribution of paclitaxel-loaded hyaluronic acid-octadecylamine carriers decreased in liver and spleen and increased in tumour tissues.36 Choi encapsulated irinotecan in hyaluronic acid nanoparticles, which was effective in inhibiting the growth of CT29 tumours of human colon carcinoma in nude mice and reducing the adverse effects of irinotecan. The metastasis of CT26 tumour of human colon cancer could be observed by fluorescence technology[37] .Zhang et al. used ciprofloxacin and vancomycin coupled with hyaluronic acid to prepare delayed-release particles of antibiotics, which could effectively inhibit Pseudomonas aeruginosa, Staphylococcus aureus and Bacillus subtilis within one week[38] .
2 Other studies
2.1 Effect on bacteria
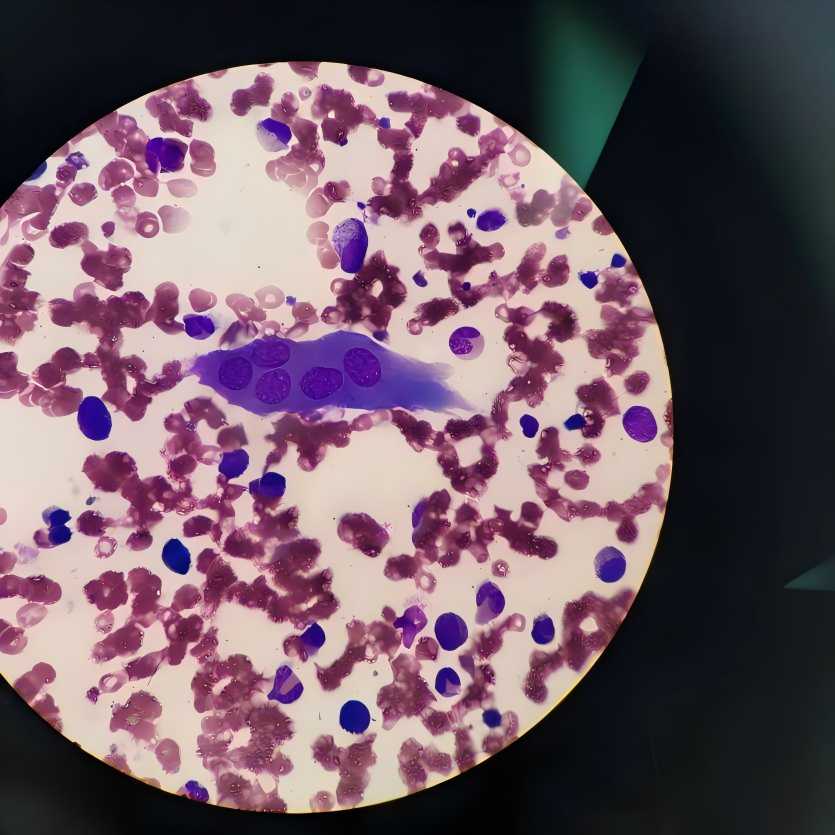
Hyaluronic acid in human body is mainly decomposed by hyaluronanolytic enzymes (Hyals), of which the most important enzymes are Hyal-1 and Hyal-2. Hyal-2 degrades hyaluronic acid into low molecular weight hyaluronic acid, and Hyal-1 degrades hyaluronic acid into low molecular weight oligomers. High molecular weight hyaluronic acid is degraded slowly by exposing only the β1 and 4 bonds. When the molecular weight of hyaluronic acid is less than 300,000 molecules, the aggregation ability of hyaluronic acid decreases and the rate of degradation increases exponentially [39]. It has been reported[40] that hyaluronic acid can be degraded to polysaccharides, which can provide nutrients for staphylococci and streptococci.
Zhang et al[41] showed that several virulence factors such as M1 protein, collagen-like surface protein and glycolytic enzyme glyceraldehyde-3-phosphate dehydrogenase of Streptococcus pyogenes were up-regulated in hyaluronic acid-rich medium. However, it has been reported [42-43] that hyaluronic acid can inhibit the growth of bacteria such as SA, with a maximum inhibitory effect achieved at a concentration of 1 mg/ml, but no bactericidal effect. High concentrations of high molecular weight hyaluronic acid inhibited the growth of SA and Escherichia coli in vitro and did not affect the efficacy of antibiotics in vitro and in vivo [28]. Jae used mouse cecum ligation and puncture method to construct a mouse abdominal abscess model, and the injection of high molecular weight hyaluronic acid (20 mg/kg) into the abdominal cavity could effectively reduce the bacterial load in the abdominal cavity, lower the level of inflammatory factors, and improve the survival rate of mice [44].

2.2 Tumour effects
Endogenous low molecular weight hyaluronic acid can promote angiogenesis, increase the blood supply of tumour cells and promote the growth of tumour cells [45-47]; in addition, endogenous low molecular weight hyaluronic acid can also promote the secretion of CD44 on the surface of tumour cells, thus promoting the metastasis of tumour cells [48]. Inhibition of hyaluronan synthase 3 (hyaluronan S3) reduces the production of low molecular weight hyaluronan, which can reduce prostate tumour angiogenesis by 70% to 80% and reduce tumour growth [49]. Overexpression of hyaluronan synthase 2 (hyaluronan S2) increases the synthesis of high molecular weight hyaluronan and increases the concentration of high molecular weight hyaluronan in tissues, which in turn inhibits the growth of tumour cells[50] . It has also been reported that endogenous hyaluronic acid can promote the proliferation and spread of tumour cells[51-53] . Exogenous hyaluronic acid has different applications depending on its molecular weight[32,54] (Table 2). When exogenous high molecular weight hyaluronic acid enters the human body, it will promote the high expression of hyaluronan S2, accelerate the synthesis of endogenous high molecular weight hyaluronic acid, increase the concentration of high molecular weight hyaluronic acid in the body, and thus inhibit tumour growth and proliferation [55].
Aikaterini used exogenous high molecular weight hyaluronic acid to significantly inhibit the migration of HT1080 cells, and when hydrolysed by hyaluronate lysozyme, the motility of HT1080 cells was significantly increased [56]. High molecular weight sodium hyaluronate gel was able to inhibit the metastasis of colon cancer cells [57]. In addition to combining with antitumour drugs, exogenous oligomeric hyaluronic acid alone can bind to CD44 receptor and enhance apoptosis of tumour cells [58], and bind to hyaluronic acid-mediated motility receptor and reduce metastasis of tumour cells [59].
3 Conclusion
The structure and function of hyaluronic acid have led to its use in biomaterials, drug-targeting agents, cosmetic surgery, and the prevention of adhesions after abdominal surgery, etc. However, with the emergence of doubts about the potential of hyaluronic acid to promote the growth and metastasis of tumour cells as well as the growth of bacteria, the use of hyaluronic acid in the clinical setting has become a matter of great caution.
In this paper, the clinical application of hyaluronic acid and the mechanism of hyaluronic acid on tumour and bacteria are reviewed, which is of great significance for the safe use of hyaluronic acid in the clinic, especially for the prevention of adhesion after abdominal and pelvic tumour patients, but the mechanism of hyaluronic acid is still needing to be further researched.
Reference
[1]MEYER K, PALMER J W. The polysaccharide of the vitreous humor[J]. J Biol Chem,1934,107(3):629-634.
[2]KOGAN G, SOLTÉS L, STERN R, et al. Hyaluronic acid: a natural biopolymer with a broad range of biomedical and indus- trial applications[J]. Biotechnol Lett,2007,29(1):17-25.
[3]EVANKO S P, TAMMI M I, TAMMI R H, et al. Hyaluronan- dependent pericellular matrix[J]. Adv Drug Deliv Rev,2007, 59(13):1351-1365.
[4]LAURENT T C, FRASER J R. Hyaluronan[J]. FASEB J,1992,6(7):2397-2404.
[5] Huang Xiaozhong, Guan Guoqiang. Research progress on the physiological functions of hyaluronic acid and its applications [J]. Animal Husbandry and Feed Science, 2015, 36 (1): 21-25.
[6] Tao Guoshu. Pharmacoepidemiology and monitoring of adverse drug reactions [J]. Chinese Journal of Geriatrics, 2005 (12): 927-928.
[7] GIRISH K S, KEMPARAJU K. The magic glue hyaluronan and its eraser hyaluronidase: a biological overview [J]. Life Sci, 2007, 80(21): 1921-1943.
[8] Chen Chao, Sun Hong, He Peihong, et al. Safety differences between different varieties of fluoroquinolone drugs [J]. Journal of Adverse Drug Reactions, 2004, 6 (5): 289-293.
[9] Corneal Disease Group of Ophthalmology Branch of Chinese Medical Association. Expert consensus on clinical diagnosis and treatment of dry eye (2013) [J]. Chinese Journal of Ophthalmology, 2013, 49 (1): 73-75.
[10] Yu Huiling. Clinical observation on the treatment of dry eye syndrome with 0.3% sodium hyaluronate and pranoprofen [J]. Electronic Journal of Clinical Medicine, 2019, 6 (60): 71.
[11] Zhong Yuankui, Liang Fang. Analysis of the cosmetic effect of micro-plastic surgery reshaping the female maxillofacial contour by fixed-point injection of botulinum toxin A into the masseter muscle combined with hyaluronic acid chin augmentation injection [J]. Chinese and foreign women's health research, 2020 (13): 112-113.
[12]SCHWARTZ S R, HAMMON K A, GAFNER A, et al. Novel hydrolyzed chicken sternal cartilage extract improves facial epi- dermis and connective tissue in healthy adult females: a ran- domized, double-blind, placebo-controlled trial[J]. Altern Ther Health Med,2019,25(5):12-29.
[13]ESPINOZA L, VINSHTOK Y, MCCREESH J, et al. Kinetic energy-assisted delivery of hyaluronic acid for skin remodeling in middle and lower face[J]. J Cosmet Dermatol,2020,19(9): 2277-2281.
[14]SCHAUSS A, SCHWARTZ S, HAMMON K, et al. The effects of skin aging associated with the use of BioCell collagen: a ran- domized, double-blind, placebo-controlled clinical trial (P06- 122-19)[J]. Curr Dev Nutr, 2019, 3(Supplement_ 1): DOI: 10.1093/ cdn/nzz031.p06-122-19.
[15] Xue Zihan, Lu Di, Li Guizhen, et al. Filling the root of facial ligaments with hyaluronic acid to improve mild to moderate facial aging [J]. Chinese Journal of Aesthetic Medicine, 2019, 28(3): 1-4.
[16]AMIRLAK B, MAHEDIA M, SHAH N. A clinical evaluation of efficacy and safety of hyaluronan sponge with vitamin C versus placebo for scar reduction[J]. Plast Reconstr Surg Glob Open,2016,4(7):e792.
[17]GUTOWSKI K A. Hyaluronic acid fillers: science and clinical uses [J]. Clin Plast Surg,2016,43(3):489-496.
[18]XIAO S, WAN Y, ZOU F, et al. Prevention of intrauterine ad- hesion with auto-crosslinked hyaluronic acid gel: a prospective, randomized, controlled clinical study[J]. Zhonghua Fu Chan Ke Za Zhi,2015,50(1):32-36.
[19]PATEL T, TEVET O. Effective treatment of acne scars using pneumatic injection of hyaluronic acid[J]. J Drugs Dermatol, 2015,14(1):74-76.
[20]CAI Z X, ZHANG H B, WEI Y, et al. Shear-thinning hyaluron- an-based fluid hydrogels to modulate viscoelastic properties of osteoarthritis synovial fluids[J]. Biomater Sci,2019,7(8): 3143-3157.
[21]ITANO N, SAWAI T, YOSHIDA M, et al. Three isoforms of mammalian hyaluronan synthases have distinct enzymatic prop- erties[J]. J Biol Chem,1999,274(35):25085-25092.
[22]HERMANS J, BIERMA-ZEINSTRA S M A, BOS P K, et al. The effectiveness of high molecular weight hyaluronic acid for knee osteoarthritis in patients in the working age: a randomised controlled trial[J]. BMC Musculoskelet Disord,2019,20(1): 196.
[23]IALENTI A, DI ROSA M. Hyaluronic acid modulates acute and chronic inflammation[J]. Agents Actions,1994,43(1-2):44- 47.
[24] Yuan Shuyan, Fu Qingpeng, Deng Xiaoqiang. Efficacy of sodium hyaluronate in the treatment of knee osteoarthritis [J]. The Great Doctor, 2019, 4(2): 108-109.
[25]PARK S H, PARK J Y, JI Y B, et al. An injectable click-cross- linked hyaluronic acid hydrogel modified with a BMP-2 mimet- ic peptide as a bone tissue engineering scaffold[J]. Acta Bioma- ter,2020,117:108-120.
[26]YANG J, ZHAO R, FENG Q, et al. Development of a carrier system containing hyaluronic acid and protamine for siRNA de- livery in the treatment of melanoma[J]. Invest New Drugs, 2021,39(1):66-76.
[27]ZHANG Y, LIU Q, YANG N, et al. Hyaluronic acid and oxid- ized regenerated cellulose prevent adhesion reformation after adhesiolysis in rat models[J]. Drug Des Devel Ther,2016,10: 3501-3507.
[28] Cai T, Han H, Cao Y, et al. Anti-adhesion effect of medical sodium hyaluronate gel and its influence on wound healing and antibiotic action [J]. Pharmaceutical Service and Research, 2020, 20(2): 92-97.
[29]LEE J W, PARK J Y, PARK S H, et al. Cross-linked electro- spun cartilage acellular matrix/poly(caprolactone-co-lactide-co- glycolide) nanofiber as an antiadhesive barrier[J]. Acta Bioma- ter,2018,74:192-206.
[30]PAŞCALĂU V, TERTIS M, PALL E, et al. Bovine serum albu- min gel/polyelectrolyte complex of hyaluronic acid and chitosan based microcarriers for Sorafenib targeted delivery[J]. J Appl Polym Sci,2020,137(34):49002.
[31]MANSOORI B, MOHAMMADI A, ABEDI-GABALLU F, et al. Hyaluronic acid-decorated liposomal nanoparticles for tar- geted delivery of 5-fluorouracil into HT-29 colorectal cancer cells[J]. J Cell Physiol,2020,235(10):6817-6830.
[32] Yang Guilan, Guo Xueping, Luan Yihong. Application of sodium hyaluronate with different relative molecular masses [J]. Food and Drugs, 2005, 7 (12): 1-3.
[33]LEE H, MOK H, LEE S, et al. Target-specific intracellular de- livery of siRNA using degradable hyaluronic acid nanogels[J]. J Control Release,2007,119(2):245-252.
[34]LEE H, LEE K, PARK T G. Hyaluronic acid-paclitaxel conjug- ate micelles: synthesis, characterization, and antitumor activity[J]. Bioconjugate Chem,2008,19(6):1319-1325.
[35]BAJAJ G, KIM M R, MOHAMMED S I, et al. Hyaluronic acid- based hydrogel for regional delivery of paclitaxel to intraperi- toneal tumors [J]. J Control Release,2012,158(3):386-392.
[36]LIU X, LIU H, WANG S L, et al. Hyaluronic acid derivative- modified nano-structured lipid carrier for cancer targeting and therapy[J]. J Zhejiang Univ Sci B,2020,21(7):571-580.
[37]CHOI K Y, JEON E J, YOON H Y, et al. Theranostic nano- particles based on PEGylated hyaluronic acid for the diagnosis,therapy and monitoring of colon cancer [J]. Biomaterials,2012, 33(26):6186-6193.
[38]ZHANG Z, SUNER S S, BLAKE D A, et al. Antimicrobial activity and biocompatibility of slow-release hyaluronic acid- antibiotic conjugated particles[J]. Int J Pharm,2020,576: 119024.
[39]STERN R, JEDRZEJAS M J. Hyaluronidases: their genomics, structures, and mechanisms of action[J]. Chem Rev,2006, 106(3):818-839.
[40]COSTAGLIOLA C, DEL PRETE A, WINKLER N R, et al. The ability of bacteria to use Na-hyaluronate as a nutrient[J]. Acta Ophthalmol Scand,1996,74(6):566-568.
[41]ZHANG M, MCDONALD F M, STURROCK S S, et al. Group A Streptococcus cell-associated pathogenic proteins as revealed by growth in hyaluronic acid-enriched media[J]. Proteomics, 2007,7(9):1379-1390.
[42]PIRNAZAR P, WOLINSKY L, NACHNANI S, et al. Bacterio- static effects of hyaluronic acid[J]. J Periodontol,1999,70(4): 370-374.
[43]CARLSON G A, DRAGOO J L, SAMIMI B, et al. Bacteriostat- ic properties of biomatrices against common orthopaedic patho- gens[J]. Biochem Biophys Res Commun,2004,321(2):472- 478.
[44]LEE J H, LIU A R, PARK J H, et al. Therapeutic effects of hya- luronic acid in peritonitis-induced Sepsis in mice[J]. Shock, 2020,54(4):488-497.
[45]THEOCHARIS A D, VYNIOS D H, PAPAGEORGAKO- POULOU N, et al. Altered content composition and structure of glycosaminoglycans and proteoglycans in gastric carcinoma[J]. Int J Biochem Cell Biol,2003,35(3):376-390.
[46]GARCÍA I, VIZOSO F, SUÁREZ C, et al. Relationship of tumoral hyaluronic acid and cathepsin D contents with histolo- gical type of gastric carcinoma[J]. Int J Biol Markers,2000, 15(3):215-218.
[47]LLANEZA A, VIZOSO F, RODRÍGUEZ J C, et al. Hyaluronic acid as prognostic marker in resectable colorectal cancer [J]. Br J Surg,2000,87(12):1690-1696.
[48]SUGAHARA K N, MURAI T, NISHINAKAMURA H, et al. Hyaluronan oligosaccharides induce CD44 cleavage and pro- mote cell migration in CD44-expressing tumor cells[J]. J Biol Chem,2003,278(34):32259-32265.
[49]SIMPSON M A, WILSON C M, MCCARTHY J B. Inhibition of prostate tumor cell hyaluronan synthesis impairs subcu- taneous growth and vascularization in immunocompromised mice[J]. Am J Pathol,2002,161(3):849-857.
[50]ITANO N, SAWAI T, ATSUMI F, et al. Selective expression and functional characteristics of three mammalian hyaluronan synthases in oncogenic malignant transformation[J]. J Biol Chem,2004,279(18):18679-18687.
[51]TOOLE B P. Hyaluronan in morphogenesis[J]. Semin Cell Dev Biol,2001,12(2):79-87. [52]BHARADWAJ A G, RECTOR K, SIMPSON M A. Inducible hyaluronan production reveals differential effects on prostate tu- mor cell growth and tumor angiogenesis[J]. J Biol Chem, 2007,282(28):20561-20572.
[53]TAMMI R H, KULTTI A, KOSMA V M, et al. Hyaluronan in human tumors: pathobiological and prognostic messages from cell-associated and stromal hyaluronan[J]. Semin Cancer Biol, 2008,18(4):288-295.
[54] Huang Yueshan, Pan Yiming, Xue Jing. Research on the function and application of hyaluronic acid with different relative molecular weights [J]. Dialysis and Artificial Organs, 2010, 21 (4): 22-25.
[55] Guo QY, Ye RY, Huang WS, et al. Effect of hyaluronic acid of different molecular weights on the expression of hyaluronic acid synthase mRNA in human peritoneal mesothelial cells. Chinese Journal of Integrative Chinese and Western Medicine Nephrology, 2002, 3(6): 320-322, 331.
[56]BERDIAKI A, NIKITOVIC D, TSATSAKIS A, et al. bFGF in-duces changes in hyaluronan synthase and hyaluronidase isoform expression and modulates the migration capacity of fibrosarcoma cells[J]. Biochim Biophys Acta,2009,1790(10): 1258-1265.
[57] Cai T, Yang W, Cao Y, et al. Experimental study on the effect of medical sodium hyaluronate gel on tumor growth and metastasis [J]. Journal of Pharmacy Practice, 2020, 38(2): 129-134.
[58]GHATAK S, MISRA S, TOOLE B P. Hyaluronan oligosaccharides inhibit anchorage-independent growth of tumor cells by suppressing the phosphoinositide 3-kinase/Akt cell survival pathway[J]. J Biol Chem,2002,277(41):38013-38020.
[59]HALL C L, LANGE L A, PROBER D A, et al. pp60(c-src) is required for cell locomotion regulated by the hyaluronanrecept- or RHAMM[J]. Oncogene,1996,13(10):2213-2224.


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese





