What You Need to Know About the Uses of Hyaluronic Acid?
Hyaluronic acid (HA) is a major component of the natural cell matrix and is widely found in related tissues such as the skin, the vitreous humour of the eye and synovial fluid [1].
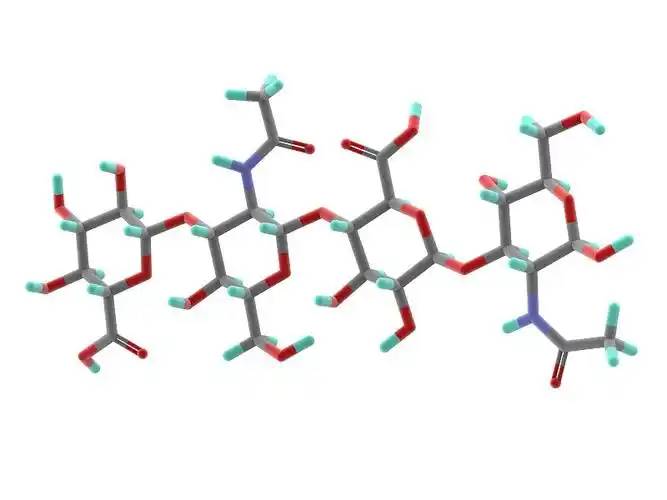
In 1934, Professors Meyer and Palmer of Columbia University in the United States [2] successfully isolated hyaluronic acid from the vitreous humour of cattle eyes for the first time. Hyaluronic acid has a linear macromolecular acidic mucopolysaccharide chemical structure, consisting of repeating disaccharide units linked by b-(1-3) glycosidic bonds between D-glucuronic acid and N-acetyl-D-glucosamine, with each disaccharide unit linked to another via a b-(1-4) glycosidic bond [3].
1. Physicochemical characteristics of hyaluronic acid
Hyaluronic acid is a white, amorphous solid that is easily soluble in water, insoluble in organic solvents, and highly hygroscopic. It is an excellent natural moisturising factor [4]. Secondly, hyaluronic acid degrades very quickly, and lymphatic tissue will degrade the hyaluronic acid injected into the tissue into carbon dioxide and water. Finally, hyaluronic acid is non-antigenic and can be found in any living organism, with no species or tissue differences.
The molecular structure of hyaluronic acid is shown in Figure 1. There are four chemical modification sites in the hyaluronic acid molecule, as shown in Figure 2: carboxyl groups, hydroxyl groups, N-acetyl amino groups and the reduced end. The hydroxyl group and the carboxyl group are commonly used modification sites. There are three ways to modify the modification sites of hyaluronic acid to improve its properties: (1) cross-linking, hydrophobisation, grafting and ring-opening chemical modifications such as esterification, reductive amination, etc. Chemical modifications such as cross-linking, hydrophobisation, grafting and ring-opening can be achieved through these reaction processes, resulting in functional hyaluronic acid derivatives such as hyaluronic acid-based gels. 2. Complexes can be formed with cationic compounds through electrostatic interactions. 3. Blending with other macromolecules can modify hyaluronic acid, and the hydrogen bonding between molecules can be used to form a blend film with excellent properties [5].
2. Applications of hyaluronic acid
Hyaluronic acid's excellent biocompatibility, water absorption, viscoelasticity, non-antigenicity and non-toxicity upon degradation mean that it can be used in a number of fields, including ophthalmology, surgery, rheumatology and urology. It can also be used to treat inflammation, improve multi-drug resistance, assist in vascular regeneration, prevent tumourigenesis and alter the viscoelasticity of the extracellular matrix.
2.1 Ophthalmology
High-concentration hyaluronic acid has the characteristics of good viscoelasticity, weak fluidity and a molecular barrier. Using these characteristics, hyaluronic acid can be used in anterior and posterior segment ophthalmic surgery, including intracapsular/extracapsular cataract extraction, intraocular lens implantation, corneal transplantation, glaucoma filtering surgery and retinal reattachment surgery, and also used as a filling substitute in vitrectomy and retinal detachment surgery. Hyaluronic acid is also the main ingredient in eye drops (for dry eye syndrome), which can effectively prolong the tear film rupture time, reduce the number of blinks in patients with dry eye syndrome, and relieve dryness, irritation, itchiness and pain symptoms [7].

From 2014 to July 2017, a total of 8 ophthalmic products containing hyaluronic acid were registered with the China Food and Drug Administration (hereinafter referred to as the ‘CFDA’), including 7 domestically produced medical devices and 1 imported medical device. The registered products are mainly used as viscoelastic protective agents. This shows that the current main application of hyaluronic acid in ophthalmology is as a viscoelastic protective agent, and research into other applications needs to be further expanded and deepened.
2.2 Surgery
Hyaluronic acid is often used in surgery to prevent or reduce postoperative adhesion in abdominal (pelvic) cavity surgery. The anti-adhesion function is due to the spatial blocking effect of hyaluronic acid, and the mechanism of action is mainly [8]: ① physically separating tissues and shielding inflammatory mediators and bacteria; ② promoting plasminolysis and, by stimulating CD44 receptor expression, promoting mesenchymal cell proliferation; ③ regulating collagen synthesis, enhancing macrophage activity, reducing fibrin deposition, promoting wound healing and reducing scar formation; ④ forming a protective film on the tissue surface, which can reduce mechanical damage, lubricate the surface and moisturise it; ⑤ absorbing and expanding to compress bleeding points, which can inhibit bleeding.
From 2014 to July 2017, four hyaluronic acid surgical medical device products were registered with the CFDA, all of which are used to prevent or reduce postoperative adhesion in abdominal (pelvic) cavity surgery. An analysis of these four products reveals the following areas that require continued, in-depth research: (1) based on research reports that hyaluronic acid sodium may be involved in the spread of tumour cells and the clinical tumour factors involved in abdominal and pelvic cavity surgery, research should be conducted to determine whether the product promotes the growth, proliferation and migration of tumour cells; (2) formulation, dosage-safety and formulation, dosage-effectiveness studies should be conducted; (3) for the indications, research should be conducted to assess whether the product interferes with the desired healing process, whether it blocks the spread of antibiotics and promotes bacterial growth and reproduction. The uncertainty of the above issues means that the effectiveness of hyaluronic acid in preventing adhesion cannot be intuitively determined, which to some extent limits the accuracy of its application in the surgical field.
2.3 Joints
Hyaluronic acid exists in the form of sodium salt in synovial fluid and is one of the components of cartilage matrix. It can lubricate the joint cavity, reduce the friction of connective tissue, and buffer the compressive effect of external forces on articular cartilage. Injecting exogenous high-molecular-weight, high-concentration, high-viscoelastic hyaluronic acid into the joint can restore the synovial fluid to a normal state and promote the natural repair of cartilage. The relatively short half-life of hyaluronic acid in the body means that frequent injections are required to treat joint lesions, which increases the suffering of patients. Jordan et al. [9] reported in 2015 on a novel gel composed of a mixture of hyaluronic acid and chitosan, which, due to the addition of chitosan, enhances the anti-degradation ability and therapeutic effect of hyaluronic acid. This study provides a new direction for improving hyaluronic acid viscous supplements for the treatment of joint lesions.

2.4 Cosmetic surgery
Hyaluronic acid has good biocompatibility, hydrophilicity and reversibility (injected hyaluronic acid can be broken down by hyaluronidase), but natural hyaluronic acid is less stable, prone to degradation and has too strong a hydrophilicity. Hyaluronic acid can be modified to develop hyaluronic acid with better biological activity and functionality, and the modified hyaluronic acid can be used as a tissue filler to replace the dermal tissue volume loss caused by aging.
Hyaluronic acid was approved for use as a soft tissue filler in Canada and Europe in 1997. The US Food and Drug Administration (FDA) did not approve such products until 2003, and the commercial name is Restylane, which contains 1% cross-linked hyaluronic acid. There are four common preparations of Restylane: Restylane Fineline, Restylane, Restylan Perlane, and Restylane SubQ. Restylane is currently the only approved preparation on the Chinese market.
From 2014 to July 2017, a total of 19 hyaluronic acid filler products were registered with the CFDA, including 11 domestically produced medical devices and 8 imported medical devices. Analysis of these 19 products found that the cross-linking agent in all registered products is BDDE, and the intended use is to inject into the middle to deep layers of facial dermal tissue to correct moderate to severe nasolabial folds. This fully demonstrates that the application of hyaluronic acid in plastic surgery is relatively mature, and a mature cross-linking agent has been formed and its use has been established. With the continuous development of the national economy and people's increasing emphasis on appearance, the plastic and cosmetic industry is bound to flourish. The future of hyaluronic acid in non-surgical cosmetic injections is therefore very promising.

2.5 Wound repair
Research by Gencer et al. [10-11] shows that hyaluronic acid can reduce the severity of inflammation and can be used as an anti-inflammatory agent. Research by NCI et al. [12] shows that hyaluronic acid can be used to treat pain after tonsillectomy. In addition, hyaluronic acid can be used to relieve pain, repair wounds [13], arthritis, tendon diseases [14], surgical treatment of deep wounds [15], burns, partial deep burns [16], surgical wounds in epithelial tissue, and chronic wounds [17].
Thiolated hyaluronic acid scaffolds cultured with adipose stem cells have been considered an ideal substitute for fat in tissue engineering. Cross-linked hyaluronic acid biomaterials have been shown to be effective in treating wounds in animal experiments on cats, dogs and horses. In wound repair and skin regeneration, hyaluronic acid can inhibit tissue adhesion and scar formation. The main roles played by hyaluronic acid in the wound healing process are [18]: (1) forming a clot with fibrin to provide structural support during wound healing; (2) regulating the inflammatory response by promoting the phagocytic activity of granulocytes; and (3) regulating collagen synthesis.
Between 2014 and July 2017, six hyaluronic acid wound repair products were registered with the CFDA, mainly for promoting wound healing and skin repair, secondary skin damage in the later stages of skin inflammation, repairing damage to the skin and mucous membranes, protecting and caring for the skin after minimally invasive surgery, and protecting skin with damaged barriers. It has the effect of maintaining skin moisture, promoting the skin's absorption of nutrients, shortening the course of the disease, reducing post-inflammatory pigmentation and scarring, treating early post-operative hyperpigmentation and reducing scarring.

2.6 Tissue engineering and regenerative medicine [19]
Tissue engineering uses biomaterials or biological scaffolds based on hyaluronic acid to enhance the efficacy of regenerative medicine. Regenerative medicine mainly refers to diseases of vital organs, controlled drug release, growth factors and antibodies, facial or intradermal implants. Hyaluronic acid has become the most suitable biopolymer for tissue regeneration medicine [20-21].
2.6.1 Hyaluronic acid scaffolds in cartilage repair
The sulfated hyaluronic acid polymer helps to improve the biocompatibility of organic/inorganic composite materials, potentially stimulating the anabolic activity of tendons, cartilage, bone and spine, restoring mesenchymal stem cells at the injury site, and also promoting the differentiation of target cells. Hyaluronic acid hydrogels can also be used in cartilage repair based on stem cell therapy. However, hyaluronic acid scaffolds still have their limitations, namely that they induce a foreign body reaction when implanted in the body. Various proteins can adsorb to the surface of implanted hyaluronic acid scaffolds and induce a range of reactions including degeneration. Non-specific proteins may be the main cause of the foreign body reaction. The adhesion of phagocytes (monocytes, leukocytes and platelets) to the surface of the hyaluronic acid scaffold may lead to the release of cytokines and inflammatory mediators in the target cells and cause inflammation.
2.6.2 Hyaluronic acid in nanomedicine
Nanoparticles made from hyaluronic acid and chitosan have been used for gene delivery in the cornea and conjunctiva [22]. Hyaluronic acid-chitosan nanoparticles carrying plasmid DNA can increase the secretion of alkaline phosphatase in human corneal epithelial tissue. Hyaluronic acid-collagen nanoparticles can successfully penetrate the epithelial cells of the cornea and conjunctiva of rabbits and transfer DNA, achieving significant transfection levels. Hyaluronic acid-collagen nanoparticles can therefore be used for gene therapy of various eye diseases, which is different from modified hyaluronic acid transport [23].
2.6.3 Hyaluronic acid in human pathophysiology
Immune surveillance, angiogenesis, malignant transformation, inflammation, multidrug resistance, tissue repair and the viscoelasticity of the extracellular matrix are all related to hyaluronic acid [24-25]. An imbalance of hyaluronic acid caused by an abnormality of hyaluronic acid synthase or hyaluronidase can lead to pathological conditions including abnormal cell proliferation, tumour metastasis and mucopolysaccharidoses [26]. The chain length, molecular weight and synthesis conditions of hyaluronic acid determine the cell response to hyaluronic acid and are expressed through the receptor cells.
2.6.4 Hyaluronic acid for tissue engineering
Hyaluronic acid's good viscoelasticity, solubility and hydrophilicity make it suitable for use in drug delivery processes, and it can be used to assist in the treatment of ophthalmology, dermatology, joints and cancer. It can be used for topical and parenteral administration. For example, hyaluronic acid can form a film on the surface of the skin or cornea to protect any drugs carried by the hyaluronic acid and form a reservoir for slow drug release, thereby improving drug retention efficiency.
Hyaluronic acid biomaterials and scaffolds offer many advantages, in particular their non-allergenic and non-inflammatory properties, which set them apart from other materials such as chitosan derivatives. However, the elasticity of injected hyaluronic acid and implanted hyaluronic acid in the body depends on the ability of hyaluronic acid to resist degradation due to hyaluronidase, reactive oxygen species and nitrogen species, which can reduce the effectiveness of hyaluronic acid [27-28]. In addition, hyaluronic acid can promote cell infiltration of blood vessels and nerve fibres, and is therefore used to induce brain and nerve regeneration.
Hyaluronic acid is one of the main components of the extracellular matrix. Due to its good biocompatibility, hydrophilicity, antigenicity and lubricity, it is widely used in ophthalmology, surgery, arthritis, plastic surgery and other fields, and has shown good application potential in the field of tissue engineering. Among them, hyaluronic acid is relatively mature in the fields of ophthalmology, surgery, arthritis and wound repair, but its application in plastic surgery and tissue engineering requires the design of hyaluronic acid products to be improved according to the specific needs of each indication to improve their performance and biocompatibility.
Reference
[1] Stern R, Maibach H I. Hyaluronan in skin: aspects of aging and its pharmacologic modulation[J]. Clin Dermatol, 2008, 26 (2): 106- 122.
[2] Meyer K, Palmer J W. On glycoproteins II. The polysaccharides of vitreous humor and of umbilical cord [J]. J Biol Chem, 1934, 107: 629-633.
[3] Sudha P N, Rose M H. Beneficial effects of hyaluronic acid[J]. Adv Food Nutr Res, 2014, 72: 137-176.
[4] Liu Hui, Liu A Juan. Hyaluronic acid, the holy product in cosmetics [J]. Chemistry Teaching, 2012, (11): 72-75.
[5] Wang Juanqin. Modification and functionalisation of hyaluronic acid [D]. Wuxi: Jiangnan University, 2013.
[6] Xu Jing, Ai Ling, Bai Huiyu, et al. Research progress on hyaluronic acid modification [J]. Polymer Bulletin, 2011, 2: 78-84.
[7] Pang Suqiu, Zhou Jinsheng, Chen Qiuxia, et al. Clinical application of sodium hyaluronate [J]. Strait Pharmacy 2003, 15(4): 252.
[8] Ling Peixue, Guan Huashi. Research and application of hyaluronic acid and its derivatives in anti-adhesion [J]. Chinese Journal of Pharmacy, 2005, 40(20): 1527-1530.
[9] Kaderli S, Boulocher C, Pillet E, et al. A novel biocompatible hyaluronic acid-chitosan hybrid hydrogel for osteoarthrosis therapy[J]. Int J Pharm, 2015, 483(1-2): 158-168.
[10] Gencer Z K, zkiri S M, Okur A, et al. A comparative study on the impact of intra-articular injections of hyaluronic acid, tenoxicam and betametazon on the relief of temporomandibular joint disorder complaints[J]. J Craniomaxillofac Surg, 2014, 42(7): 1117-1121.
[11] Voigt J, Driver V R. Hyaluronic acid derivatives and their healing effect on burns, epithelial surgical wounds, and chronic wounds: a systematic review and meta analysis of randomized controlled trials[J]. Wound Repair Regen, 2012, 20(3): 317-331.
[12] Hanci D, Altun H. Effectiveness of hyaluronic acid in post- tonsillectomy pain relief and wound healing-A prospective, double- blind, controlled clinical study[J]. Int J Pediatric Otorhinolaryngol, 2015,79(9): 1388-1392.
[13] Ramos-Torrecillas J, Garcia-Martinez O, Luna-Bertos E D, et al.
Effectiveness of platelet-rich plasma and hyaluronic acid for the treatment and care of pressure ulcers[J]. Biol Res Nurs, 2015, 17 (2): 152-158.
[14] Abate M, Schiavone C, Salini V. The use of hyaluronic acid after tendon surgery and in tendinopathies[J]. Biomed Res Int, 2014, 2014: 783632.
[15] Onesti M G, Fino P, Ponzo I, et al. Non-surgical treatment of deep wounds triggered by harmful physical and chemical agents: a successful combined use of collagenase and hyaluronic acid[J]. Int Wound J, 2016, 13(1): 22-26.
[16] Dalmedico M M, Meier M J, Felix J V, et al. Hyaluronic acid covers in burn treatment: a systematic review[J]. Rev Esc Enferm USP, 2016, 50(3): 519-524.
[17] Voigt J, Driver V R. Hyaluronic acid derivatives and their healing effect on burns, epithelial surgical wounds, and chronic wounds: a systematic review and meta-analysis of randomized controlled trials[J]. Wound Repair Regen, 2012, 20(3): 317-331.
[18] Tezel A, Fredrickson G H. The science of hyaluronic acid dermal fillers[J]. J Cosmet Laser Ther, 2008, 10(1): 35-42.
[19] Hemshekhar M, Thushara R M, Chandranayaka S, et al. Emerging roles of hyaluronic acid bioscaffolds in tissue engineering and regenerative medicine[J]. Int J Biol Macromolecules, 2016, 86: 917-928.
[20] Girish K S, Kemparaju K. The magic glue hyaluronan and its eraser hyaluronidase: a biological overview[J]. Life Sci, 2007, 80(21): 1921-1943.
[21] Hogan M, Girish K, James R, et al. Growth differentiation factor-5 regulation of extracellular matrix gene expression in murine tendon fibroblasts[J]. J Tissue Eng Regen Med, 2011, 5(3): 191-200.
[22] Rivkin I, Cohen K, Kofler J, et al. Paclitaxel-clusters coated with hyaluronan as selective tumor-targeted nanovectors[J] . Biomaterials, 2010, 31 (27): 7106-7114.
[23] de la Fuente M, Seijo B, Alonso M J. Bioadhesive hyaluronan- chitosan nanoparticles can transport genes across the ocular mucosa and transfect ocular tissue[J]. Gene Ther, 2008,15 (9):668-676.
[24] Girish K S, Kemparaju K. The magic glue hyaluronan and its eraser hyaluronidase: a biological overview[J]. Life Sci, 2007, 80 (21) 1921-1943.
[25] Jiang D, Liang J, Noble P W. Hyaluronan as an immune regulator in human diseases[J]. Physiol Rev, 2011, 91 (1): 221-264.
[26] Toole B P. Hyaluronan: from extracellular glue to pericellular cue[J]. Nat Rev Cancer, 2004, 4 (7): 528-539.
[27] Prestwich G D. Hyaluronic acid-based clinical biomaterials derived for cell and molecule delivery in regenerative medicine[J] . J Control Release, 2011, 155 (2): 193-199.
[28] Schantéa C E, Zuber G, Herlin C, et al. Chemical modifications of hyaluronic acid for the synthesis of derivatives for a broad range of biomedical applications[J]. Carbohydr Polym, 2011, 85 (3) 469- 489.


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese