What Is the Use of Hyaluronic Acid in the Dentistry Field?
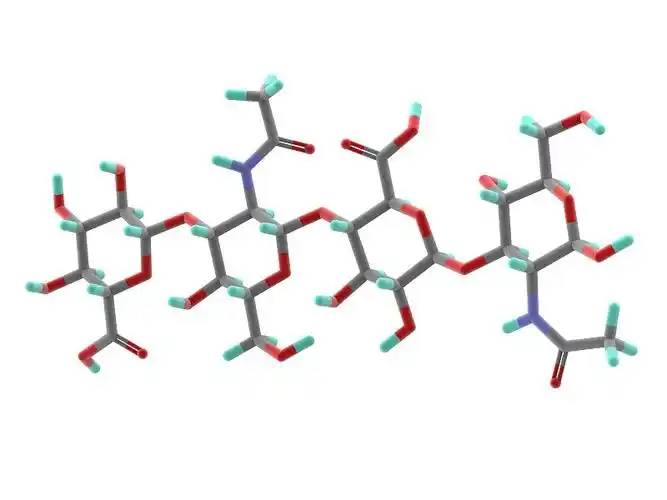
Hyaluronic acid, also known as hyaluronan, is an acidic mucopolysaccharide composed of D-glucuronic acid disaccharide units and N-acetylglucosamine [1]. It is widely distributed in the connective tissue between human cells, the vitreous body of the eye, and synovial fluid in the joints. It is an important component of the skin. Hyaluronic acid is a high-molecular polymer with an average molecular weight ranging from 100,000 to 10 million daltons (unit of mass). Its molecular structure is shown in Figure 1 [2].
The molecular structure of hyaluronic acid is surrounded by many functional groups such as hydroxyl and carboxyl groups, making it soluble in water but insoluble in organic solvents such as ethanol and ether. These functional groups make it a very strong water absorbent through hydrogen bonding and other effects. Hyaluronic acid is a white, pasty or fibrous substance with a faint odour. It is a highly absorbent substance that dissolves slowly and completely in water. It can absorb thousands of times its own molecular weight in water, which is much more than other polysaccharide compounds. Therefore, hyaluronic acid is a natural moisturiser in nature [3-4].
The application fields of hyaluronic acid are gradually expanding with further research, including medicine, cosmetics, health food and beauty injections. Despite its superior properties and wide range of applications, hyaluronic acid is limited in its use due to its complex molecular structure, which causes reactions between or within molecules, and the addition of hyaluronic acid can easily increase the viscosity and consistency of the system. This article summarises the preparation methods, special properties and influencing factors of hyaluronic acid, and describes the application fields of hyaluronic acid.
1 Preparation methods for hyaluronic acid
There are three main methods for preparing hyaluronic acid: animal extraction, microbial fermentation and chemical synthesis [5-7]. Animal extraction is currently the main method for preparing hyaluronic acid, and it can generally be extracted from fresh animal tissues such as human umbilical cords, animal glass balls, chicken combs or whale cartilage. However, the supply of raw materials is limited, which makes it expensive. In addition, the hyaluronic acid content in these raw materials is low, resulting in low yields. Coupled with the complexity of the extraction method, it is unable to meet the growing demand for research and application. In the microbial fermentation method, hyaluronic acid can be prepared by fermenting Streptococcus equi, Streptococcus zooecus, and Streptococcus equinus. This method has certain advantages over the animal tissue extraction method.
The raw materials for this method are readily available, the sources are relatively abundant, the cost is low, and the extraction process is simple and convenient. However, hyaluronidase is easily produced during the entire preparation process, so the production process needs to be well controlled. The chemical synthesis method is relatively cheaper than the previous two. It mainly synthesises ‘hyaluronic acid oxaziridine derivatives’ through polysaccharide polymers, and then adds a certain amount of decomposing enzyme. The process of precipitation, separation and purification is used to produce synthetic hyaluronic acid, which has successfully replaced natural hyaluronic acid.
2 Properties and characteristics of hyaluronic acid
Hyaluronic acid is a high-molecular polymer with active functional groups such as carboxyl groups, hydroxyl groups, N-acetyl groups and reducing ends distributed on the surface. It can not only be modified by cross-linking, esterification, grafting, molecular modification and compounding, but also form hydrogen bonds with water molecules and adsorb a large amount of water. Studies have found that 1 g of hyaluronic acid can adsorb 6 L of water, far exceeding the water adsorption capacity of other substances [8]. Therefore, hyaluronic acid is widely used as a moisturising agent in cosmetic products.
Hyaluronic acid is able to form a network structure in a solvent, changing the rheological properties of the solution. The molecular structure of hyaluronic acid has hydrophilic reactive functional groups on the surface, which spread out in a solvent, occupying a lot of space. As the concentration increases, the interactions between the intra- or intermolecular chains of these macromolecules can form a network structure, which leads to an increase in the viscosity and elasticity of the solution and causes unique rheological properties [9]. Hyaluronic acid molecules have a relatively stable molecular structure, but are sensitive to changes in ionic strength and pH in the solution [10].
Molecular diffusion often occurs in solutions with low ionic strength due to the repulsion between charges, which increases the viscosity of the solution [11]. When dilute solutions expand, hyaluronic acid molecules slowly become longer and wider in the solution, eventually forming a round substance. When the concentration of the solution exceeds 1%, hyaluronic acid can form a continuous network structure. The higher the concentration, the more serious the phenomenon of crossing and overlapping. In addition, the cross-linking and interaction between molecular chains form a double-helix structure, which makes the formed network structure more stable. The more serious the phenomenon is in hyaluronic acid molecules with high molecular weight and large molecular volume [12-13], the greater the change in the physical properties of hyaluronic acid.
Hyaluronic acid is generally used in higher-end products and added in very small amounts. This is partly due to the fact that hyaluronic acid is expensive and its sources are limited, and partly due to the properties it exhibits. Natural hyaluronic acid has a short half-life, is easily degraded and diffused, has poor stability and is overly water-soluble [14]. In addition, the active functional groups within or between hyaluronic acid molecules are prone to react in an electrolyte, causing cross-linking and overlap between the chains of the molecule itself or adjacent molecules to form a mass of material. In addition to strictly limiting the amount of hyaluronic acid added, the experiment also needs to control the dissolution process of hyaluronic acid. Its highly water-absorbent nature makes it very easy to disperse unevenly in many aqueous systems, and also increases the consistency of the system [15], making the system state difficult to control.
3 Application of hyaluronic acid
3. 1 Application in cosmetics
Due to its special molecular structure, hyaluronic acid has been widely used in cosmetics as a moisturising agent. Compared with other moisturisers, it has a better moisturising effect and is suitable for the moisturising requirements of cosmetics in different environments and humidity levels [16]. It is also non-greasy and does not block the pores of the skin. Hyaluronic acid itself is a high-molecular polymer with a strong lubricating effect and film-forming properties. Cosmetics containing hyaluronic acid feel noticeably smoother when applied, feel good on the skin and form a thin film on the skin's surface after application, giving the skin a good feeling of smoothness and moisture and protecting the epidermis.
In addition, hyaluronic acid, either alone or in combination with phospholipids, can be added to the aqueous or oily medium to emulsify the cosmetic product. This natural emulsifier is environmentally friendly and safe, and can be used in the production of food, skin creams, lotions, facial cleansers, etc. Hyaluronic acid with a molecular weight of more than 3000KD has good viscosity and can be used as a good thickener in cosmetics. Macromolecular hyaluronic acid not only forms a protective film on the surface of the substrate, but also acts as a molecular capsule to encapsulate small molecules. It is especially suitable for use in some fragrance products, combining with fragrance molecules and encapsulating them, so as to not only slow down the volatilisation of the fragrance and make it last longer, but also prevent the fragrance from coming into direct contact with the skin, causing adverse reactions such as irritation and other allergic symptoms.

In addition, hyaluronic acid itself is a component of skin tissue, regulating the diffusion and transport of proteins, water and electrolytes. Exogenous hyaluronic acid also plays a supplementary role to endogenous hyaluronic acid. Hyaluronic acid with a smaller molecular weight can penetrate into the superficial layer of the skin, supplying the skin with nutrients and excreting waste products, preventing skin ageing, playing a role in beauty and skin care, prolonging the adhesion of make-up and lipstick on the skin, etc., and is a commonly used product in some beauty salons and cosmetics production sites. Loureiro Borghetti et al. [17] studied the effect of hyaluronic acid on the mouse mouth from a clinical and histological perspective, and found that a hyaluronic acid solution at a certain concentration can stimulate collagen formation. Some scholars have found that hyaluronic acid is beneficial to tissue repair and slightly protects collagen formation. Adding a certain amount of hyaluronic acid to hair care products can also have the effect of smoothing the hair. The above shows that hyaluronic acid is a good cosmetic ingredient.
3. 2 Application in medicine
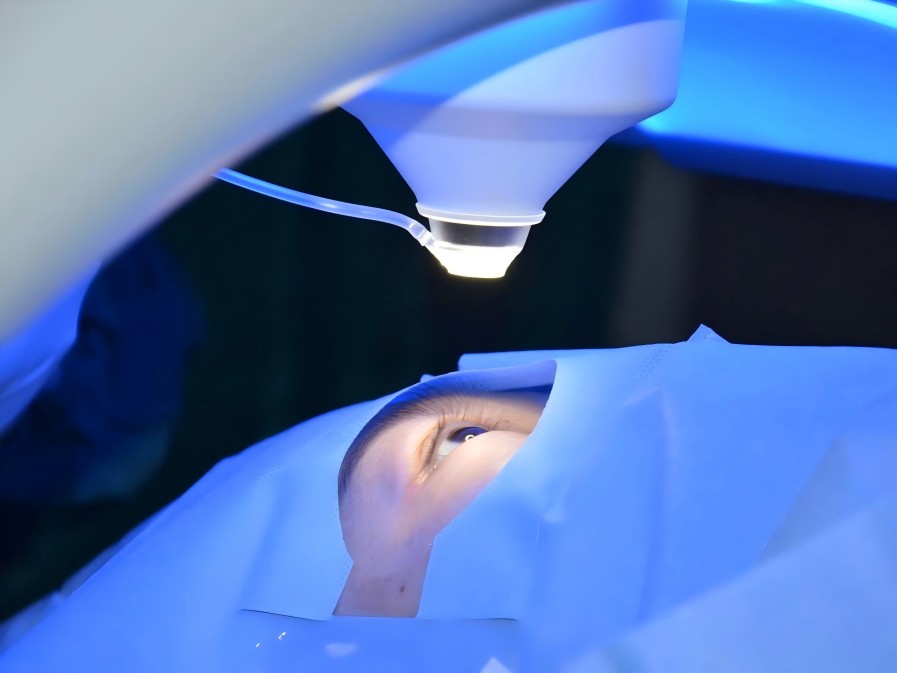
Hyaluronic acid is used in ophthalmology, rhinology, laryngology, orthopaedics and general surgery. Hyaluronic acid gel is used as a filling agent in ophthalmological operations such as extracapsular cataract extraction, intraocular lens implantation, retinal detachment and corneal transplantation. A dilute solution of hyaluronic acid is also used to treat dry keratoconjunctivitis syndrome. Hyaluronic acid's wetting and buffering effects can be used to treat symptoms such as osteoarthritis, frozen shoulder and rheumatoid arthritis. It can also be used in urology to treat interstitial cystitis and protect the bladder epithelium's glycosaminoglycan protective layer [18].
Because the outer layer of the hyaluronic acid molecule is rich in active functional groups, it can bind to many drug molecules and become a carrier that delivers various drugs to pathological sites, overcoming the problem of drugs being degraded before reaching the pathological site. Before binding to the drug molecule, hyaluronic acid needs to be cross-linked and modified, and the receptor hyaluronic acid needs to be selected to a certain extent, so that the drug can be fully located at the pathological site and slowly released, which can greatly enhance the efficacy of the drug [19]. For example, hyaluronic acid is often used to form a complex with BMP (bone morphogenetic protein), which can be injected into the affected area to slowly release BMP and exert its osteogenic effect.
3. 3 Application in the oral field
Because hyaluronic acid has antibacterial, anti-inflammatory and anti-edema effects, it has been medically proven that the application of hyaluronic acid gel can alleviate the symptoms of plaque gingivitis, a common infectious disease of the gingival tissue. Compared with the therapeutic effect of hyaluronic acid alone, the combination of scaling and root planing can more effectively improve the recovery of gingival inflammation and clinical indicators. Hyaluronic acid combined with subgingival scaling and root surface smoothing can quickly reduce the inflammatory response of periodontal tissue in patients with chronic periodontitis [20] (see Figures 3 and 4 below).
Studies have also shown that hyaluronic acid combined with guided periodontal tissue regeneration can promote alveolar bone recovery and bone mineralisation in the treatment of chronic periodontitis. Hyaluronic acid itself is a component of the extracellular matrix of periodontal connective tissue and regulates the hydration of the extracellular matrix. Hyaluronic acid with a relatively high molecular weight can also inhibit the proliferation of gingival epithelial cells, lymphocytes and fibroblasts, shorten the inflammatory process of periodontitis and improve the condition. Domestic and foreign studies have shown that after mechanical treatment of periodontitis patients or after periodontal surgery, hyaluronic acid gel can reduce periodontal tissue destruction, alleviate periodontal inflammation and promote the recovery of periodontal tissue.
Zhang Li et al. [22] found that hyaluronic acid can significantly reduce the peri-implant sulcus bleeding index and plaque index in patients with peri-implant mucositis, and is more effective than mechanical plaque and calculus removal. At the same time, some researchers have found that after mechanical plaque removal and SRP, injecting a mixed solution of a certain proportion of chlorhexidine and hyaluronic acid into the periodontal pocket significantly improves the peri-implant index, indicating that hyaluronic acid combined with chlorhexidine has a good effect on the treatment of peri-implantitis.
In addition to studies that have proven its ability to kill bacteria and prevent the formation of plaque, hyaluronic acid also has certain applications in the healing of tooth extraction wounds. Mendes et al. [23] injected relatively large molecule hyaluronic acid gel into the tooth extraction wounds of rats, and observed and analysed the tissue and morphology of the wound healing process at irregular intervals. They found that after 21 days, the amount of bone formation at the extraction site had increased, and the deposition of bone matrix and cell arrangement were more orderly. Some researchers [24] also conducted experiments on rabbits, injecting 0.8% hyaluronic acid gel into their tooth extraction sockets.
After a period of time, it was found that a large amount of alveolar bone had formed in the extraction sockets. Zeng Yunting and others analysed that this is because hyaluronidase in the extraction wound can break down hyaluronic acid with a relatively large molecular weight into small molecular hyaluronic acid to stimulate osteogenic inductive factors and promote wound healing. Lai Hanbiao et al. [25] confirmed that hyaluronic acid gel and physiological saline were used to treat 50 patients after dental implant surgery, and found that hyaluronic acid gel can significantly promote wound healing, improve redness and swelling, and reduce patient pain.
Nolan et al. [26] used 0.2% hyaluronic acid gel by mass fraction to treat recurrent aphthous ulcers, found that it could immediately relieve symptoms and promote ulcer healing. Lee et al. [27] also studied the efficacy and safety of hyaluronic acid in the treatment of recurrent aphthous ulcers and conducted a large number of clinical trials. They found that after two weeks, most patients experienced improved pain after using hyaluronic acid, nearly half of them had a reduction in the number of ulcers, and the ulcer area decreased in about 78% of patients. All of the above strongly proves that hyaluronic acid can protect the oral mucosa, resist inflammation and edema, and effectively improve various oral wounds and inflammations.
4 Summary
Hyaluronic acid is a high-molecular polysaccharide substance with a unique molecular structure that is both hydrophilic and hydrophobic. It can undergo various chemical modifications through esterification, amidation and reductive amination reactions. This environmentally friendly and safe compound has broad application prospects. First, hyaluronic acid itself has good water absorption and moisturising properties, and it is also a component of skin tissue. It can supplement the lack of endogenous hyaluronic acid, and can be used as a moisturising agent in cosmetics as well as having an anti-ageing effect. Hyaluronic acid also has antiseptic, anti-inflammatory and anti-edema effects. It can be used alone or in combination with other drugs or surgical treatments to improve symptoms such as gingivitis, periodontitis, mucositis around dental implants, wounds from tooth extraction and recurrent aphthous ulcers. As hyaluronic acid production technology improves, its use in cosmetics, pharmaceuticals and dentistry will continue to be promoted.
References
[1] Wang Jiangling, Ran Weizhi. The current situation and development trend of hyaluronic acid and its derivatives [J]. Heilongjiang Medical Science, 2014, 37 (6), 117-118
[2]Lillian C. Becker ,Wilma F. Bergfeld ,Donald V. Belsito, Curtis D. Klaasen,James G. Marks Jr ,Ronald C. Shank,Thomas J. Slaga,Paul W. Snyder,Cosmetic Ingredient Review Expert Panel,and F. Alan Andersen. Final Report of the Safety Assessment of Hyaluronic Acid ,Potassium Hyaluronate ,and Sodium Hyaluronate ,International Journal of Toxicology. Vol. 28,No. 4S,July / August 2009
[3] Wu Dongru, ed. Biochemistry of Sugars. Beijing: Higher Education Press, 1987: 627
[4] Nagai Masayoshi. Cosmetic ingredients. JP Show 62-158203, 1987
[5] Chen Zhongjie, Guo Ailing. Application and production of hyaluronic acid [J]. Henan Chemical Industry, 2007, 24, 48-49
[6]Palmieri B,Merighi A,Corbascio D,et al. Fixed combination of hyaluronic acid and chondroitin - sulphate oral formulation in randomized double blind,placebo controlled study for the treatment of symptoms in patients with non-erosive gastroesophageal reflux [J]. Eur Rev Med Pharmacol Sci,2011,17 (24) : 3272-3278
[7] Zhou Panghu, Ma Beilei, Qiu Bo, et al. Effect of hyaluronic acid/chitosan microspheres on the expression of matrix metalloproteinase and its inhibitory factor mRNA in inflammatory chondrocytes [J]. Chinese Journal of Experimental Surgery, 2013, 30(11): 2377-2379
[8]Billek G,Billek D. Hyaluronic acid : the history of an active in- gredient in cosmetics [in German][J]. Parfuem Kosmet. 1988 ; 69 : 788 - 790 ; 792-795
[9]Laurent TC,Structure of Hyaluronic Acid. New York,NY : Ac- ademic Press ; 1970
[10]Cleland RL,Wang JL,Detweiler DM,Polyelectrolyte proper- ties of sodium hyaluronate. 2 : potentiometric titration of hyaluronic acid. Macromolecules J[J]. 1982 ; 15 : 386-395
[11]Balazs EA,Laurent TC. Viscosity function of hyaluronic acid as a polyelectrolyte[J]. J Polym Sci. 1951 ; 6 :665-667
[12]Scott JE,Cummings C,Brass A,Chen Y. Secondary and tertiary structures of hyaluronan in aqueous solution ,investigated by rotary shadowing - electron microscopy and computer simulation. Biochem J [J].1991 ; 274 : 699-705
[13]Lillian C. Becker ,Wilma F. Berfeld ,Donald V. Belsito, Curtis D. Klaassen,James G. Marks Jr,Ronald C. Shank,Thomas J. Slaga,Paul W. Snyder,Cosmetic Ingredient Review Expert Panel,and F. Alan Andersen. Final Report of the Safety Assessment of Hyaluronic Acid,Potassium Hyaluronate,and Sodium Hyaluronate[J]. Internation- al Journal of Taxicology / Vol. 28,No. 4S,July / August 2009
[14]Balazs EA ,Band P. Hyaluronic acid : its structure and use. Cosmetics & Toiletries[J]. 1984 ; 99 : 65-72
[15]Scott JE. Secondary and tertiary structures of hyaluronan in a- queous solution : some biological consequences. 1988. Available at : ht- tp: / /www. glucoforum. gr. Jp / science / hyaluronan / HA02 / HA02E. html. Accessed February 21,2005
[16] Xu Hong, Lu Zhihua. Application of sodium hyaluronate in cosmetics [J]. Chinese Journal of Biopharmaceuticals, 1998, 19(5), 222-223.
[17]Ruchielli Loureiro Borghetti,Karlon Froes de Vargas,Sabrina Pozatti Moure,Fernanda Goncalves Salum,Maria Antonia Zancanaro de Figueiredo,Porto Alegre. Clinical and histologic evaluation of effects of hyaluronic acid in rat tongue[J],ORAL AND MAXILLOFACIAL SUR- GERY,2012,113 (4) ,499-494
[18] Li Yunyun, Fayonghong. Progress in the application of hyaluronic acid in the field of dentistry. International Journal of Dentistry, 2013, 40(3), 344-346.
[19]Lee JH,Jung JY,Bang D. The efficacy of topical 0. 2% hyal- uronic acid gel on recurrent oral ulcers : Comparison between recurrent aphthous ulcers and the oral ulcers of Behcet’s disease[J]. J Eur Acad Dermatol Venereol,2008,22(5) : 590-595
[20] Wu Yafei, Huang Jiao, Xu Yi, et al. The effect of Gengigel gel in the treatment of plaque gingivitis [J]. Journal of Practical Stomatology, 2005, 21 (4), 540-542
Yiyao.com. Italian cavity treatment hyaluronic acid series (HA) [EB/OL]. (2013-6-25) [2015-9-11]. http://www.eyar.com/html/new/2013/0625/1717.html
[21] Zhang Li, Chen Gang, Ma Lian, et al. Clinical study on sodium hyaluronate for the treatment of peri-implant mucositis [J]. Chinese Journal of Oral Implantology, 2005, 1, 22-24
[22]Mendes RM,Silva GA,Lima MF,et al. Sodium hyaluromate accelerates the healing process in tooth sockets of rats[J]. Arch Oral Bi- ol,2008,53 ( 12) : 1155 -1162
[23]Fawzy El-Sayed KM,Dahaba MA,Aboul-Ela S,et al. Lo- cal application of hyaluroman gel in conjunction with periodontal surgery : A randomized controlled trial[J]. Clin Oral Investig,2012 ,16 (4 ) : 1229 -1236
[24] Lai Hanbiao, Liu Yi. The role of hyaluronic acid gel in wound healing after implantation [J]. Guangdong Dental Disease Prevention and Control, 2008, 16(Suppl.): 637-638
[25]Nolan A,Baillie C,Badminton J,et al. The efficacy of topi- cal hyaluronic acid in the management of recurrent aphthous ulceration [J]. J Oral Pathol Med,2006,35 (8) : 461 - 465
[26]Lee JH,Jung JY,Bang D. The efficacy of topical 0. 2% hyal- uronic acid gel on recurrent oral ulcers : Comparison between recurrent aphthous ulcers and the oral ulcers of Behcet’s disease[J]. J Eur Acad Dermatol Venereol,2008,22(5) : 590 - 595


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese