What Is the Use of Hyaluronic Acid in the Oral Field?
Hyaluronic acid (HA) plays a crucial role in clinical applications, including moisture retention, lubrication, and regulation of osmotic pressure. It protects normal cells from toxic cells and free radicals, and stimulates cell migration, adhesion, proliferation, and differentiation [1]. With the advancement of research and the accumulation of clinical experience, hyaluronic acid has found many new applications, and its use in the oral field has gradually gained attention.
1 Application of Hyaluronic Acid in Temporomandibular Joint Disorder
Temporomandibular joint disorder (TMJD) is one of the most common conditions in the oral and maxillofacial region, characterised by symptoms such as joint noises, pain, and abnormal movement of the mandible. Intra-articular drug injection is one of the conservative treatment methods for this condition. Sodium hyaluronate (SH) is the sodium salt form of hyaluronic acid. In recent years, several studies have reported that intra-articular injection of SH can effectively treat TMJD [2-3].
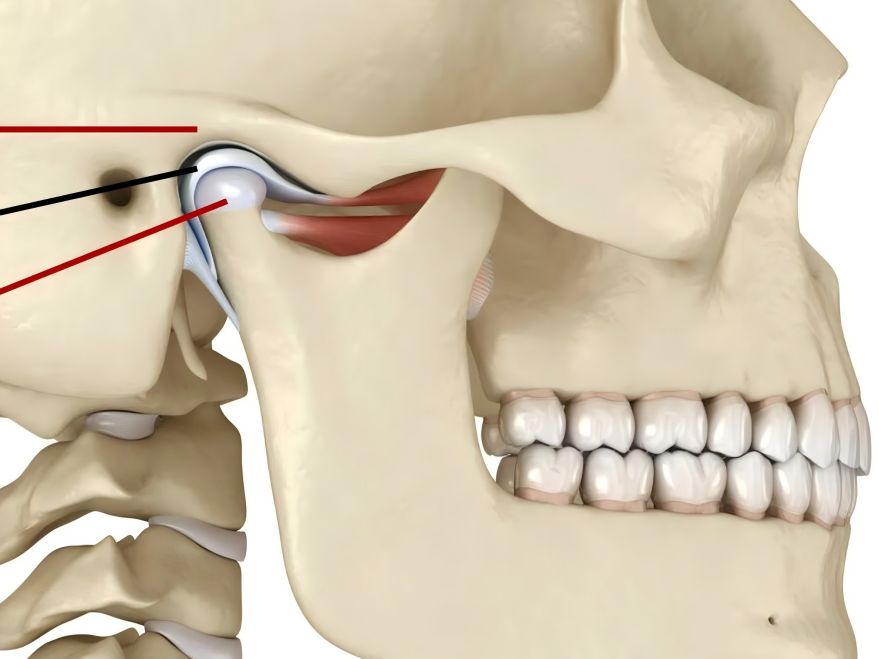
Hyaluronic acid is secreted by synovial B cells and exists in the synovial fluid and cartilage of joints in the form of sodium salts, performing functions such as lubrication, protection, and nutrition of joint structures. Li Chunjie et al. [4] conducted a systematic review of clinical randomised controlled trials evaluating SH treatment for temporomandibular joint structural disorders. They found that SH significantly improved patients' maximum mouth opening in both the short and long term, and significantly improved the overall clinical evaluation of the disease in the short term; however, its long-term effects were not significant. Compared with glucocorticoids, SH demonstrated superior short-term clinical overall evaluation and fewer adverse reactions post-injection.
Intra-articular injection of SH into the temporomandibular joint can also effectively treat temporomandibular joint osteoarthritis (TMJOA). Liu Peicai et al. [5] found in their study on the mechanism of action of SH that SH may exert its therapeutic effect on TMJOA by reducing the levels of matrix metalloproteinases-2 and 3 in the synovial fluid of patients, thereby slowing down the rate of cartilage matrix destruction in the joint. Other reports [6] have also indicated that joint lavage and intra-articular injection of SH solution after condylar fracture surgery can prevent and treat postoperative complications. The mechanism of action may involve: supplementing endogenous hyaluronic acid deficiency, restoring joint surface lubrication, regulating intra-articular viscoelasticity, improving joint mobility, and feedback regulation of the patient's own hyaluronic acid biosynthesis to eliminate pain-causing substances.
2 Application of hyaluronic acid in periodontal tissue diseases
2.1 Application of hyaluronic acid in plaque-induced gingivitis
Plaque-induced gingivitis is a chronic infectious disease of the gingival tissue, currently primarily treated through oral hygiene education and scaling. When used alone, hyaluronic acid gel can significantly alleviate gingival inflammation in plaque-induced gingivitis. Combining hyaluronic acid gel with scaling therapy for gingivitis is more effective and more beneficial for the recovery of gingival inflammation and improvement of clinical indicators compared to scaling alone [7]. Some researchers have evaluated the efficacy of locally applied hyaluronic acid gel for treating gingivitis from clinical and histopathological perspectives: due to its antibacterial, anti-inflammatory, and anti-edematous properties, hyaluronic acid improves gingival indices and reduces damage to tooth hard tissue and periodontal tissue caused by repeated scaling, whether used alone or as an adjunct to scaling.

2.2 Application of hyaluronic acid in chronic periodontitis
For the treatment of periodontitis, mechanical therapy alone can achieve good clinical outcomes for most patients. However, for a minority of patients, comprehensive treatment is required, which includes not only mechanical debridement but also adjunctive antimicrobial therapy [8]. Localised drug application, which can directly reach the affected area, has high local concentrations of antimicrobial agents, acts slowly and sustainably, and has minimal adverse effects, making it widely used in modern periodontitis treatment. Xu Yi et al. [9] found that hyaluronic acid combined with subgingival scaling and root planing (SRP) could rapidly reduce inflammatory responses in periodontal tissues of patients with chronic periodontitis, but no promotional effect on periodontal tissue repair and regeneration was observed. Other researchers [10] reported that after modified Widmann flap surgery for chronic periodontitis, local application of 0.8% hyaluronic acid gel significantly improved attachment levels and reduced gingival recession. Additionally, studies have shown that hyaluronic acid combined with guided periodontal tissue regeneration promotes alveolar bone repair and mineralisation in the treatment of chronic periodontitis.
Hyaluronic acid is an important component of the extracellular matrix of periodontal connective tissue cells and regulates the hydration of the extracellular matrix. High-molecular-weight hyaluronic acid can inhibit the proliferation of gingival epithelial cells, fibroblasts, and lymphocytes, shorten the inflammatory process of periodontitis, and improve the condition of the affected area. Since numerous studies both domestically and internationally have demonstrated that hyaluronic acid possesses anti-inflammatory, anti-infective, and tissue-regenerative properties, as well as promoting wound healing, local application of hyaluronic acid gel following mechanical therapy or periodontal surgery can prevent periodontal tissue destruction, reduce gingival inflammation, and facilitate periodontal tissue recovery in patients with chronic periodontitis.
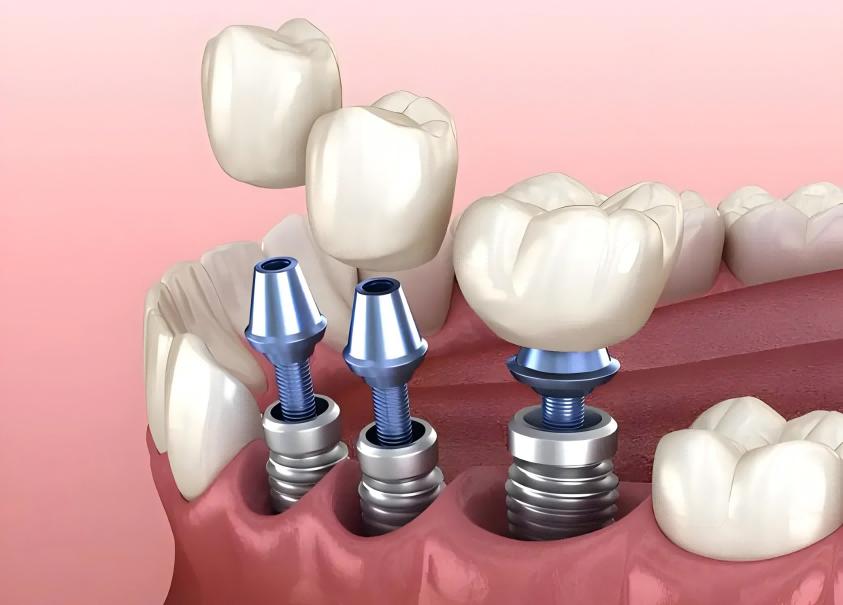
2.3 Application of Hyaluronic Acid in Peri-implantitis
Peri-implant mucositis is an early stage of peri-implantitis, with inflammation confined to the gingival mucosa around the implant, without bone resorption, and presenting clinical symptoms such as pocket formation and bleeding on probing. Zhang Li et al. [11] found that, compared with mechanical removal of plaque and calculus, the use of hyaluronic acid in patients with peri-implant mucositis resulted in a significant reduction in the peri-implant gingival sulcus bleeding index and plaque index. For peri-implantitis, due to the formation of deep peri-implant pockets and significant alveolar bone resorption, comprehensive treatment should be administered, including scaling, medication, bone grafting, membrane technology, and membrane gingivoplasty. However, whether hyaluronic acid can exert antibacterial, anti-inflammatory, and tissue regeneration and healing effects during treatment remains to be further investigated.
Some researchers have conducted exploratory studies on the treatment of peri-implantitis using non-surgical methods. After mechanically removing plaque and performing scaling and root planing (SRP), they injected a solution containing 0.2% chlorhexidine and 0.8% hyaluronic acid into the pocket. Compared with pre-treatment levels, the peri-implant index improved significantly in all groups, and there were no significant differences between groups. They concluded that hyaluronic acid and chlorhexidine have similar efficacy when combined with mechanical methods for treating peri-implantitis.

3 Application of hyaluronic acid in wound healing
3.1 Application of hyaluronic acid in tooth extraction wound healing
The healing of extraction wounds is influenced not only by systemic and local factors such as physical and chemical conditions, hormones, and medications but also by a series of growth factors, including osteopontin (OPN), bone morphogenetic protein (BMP)-2, and vascular endothelial growth factor (VEGF).
Mendes et al. [12] injected high-molecular-weight hyaluronic acid gel into rat tooth extraction sites and analysed the histological and morphological changes during the healing process. They found that by day 7 post-extraction, the number of trabecular bones in the apical and middle thirds of the root was significantly increased; by day 21 post-extraction, in addition to an increase in the number of trabecular bones, bone matrix deposition and cell arrangement were more ordered; simultaneously, within 2–7 days post-extraction, the overall expression of OPN and BMP-2 in the extraction site was enhanced, with particularly prominent expression in the apical 1/3 region.
Researchers studying the healing process of rabbit extraction sockets found that, compared to the blank control group, the group injected with 0.8% hyaluronic acid gel into the extraction socket exhibited earlier and more abundant alveolar bone formation within the socket. Based on this, Zeng Yunting et al. [13] concluded that: Hyaluronidase in the extraction socket breaks down high-molecular-weight hyaluronic acid into low-molecular-weight hyaluronic acid, which stimulates bone formation-inducing factors to promote wound healing; simultaneously, hyaluronic acid also stimulates the migration and proliferation of endothelial cells, thereby promoting angiogenesis, increasing the number of osteoblasts from blood vessels, and enhancing bone formation.
3.2 Application of hyaluronic acid in the healing of implant wounds
Lai Hanbiao et al. [14] conducted a randomised double-blind study on 50 patients who underwent dental implant surgery, comparing the effects of hyaluronic acid gel and saline solution on wound healing. The results showed that hyaluronic acid gel significantly promoted wound healing, particularly during the early stage of wound healing (on the 3rd day). Hyaluronic acid can significantly reduce wound redness and swelling, thereby alleviating patients' pain responses. This is attributed to the role of hyaluronic acid salts in wound repair, including wound cleansing, anti-inflammatory effects, and promotion of wound healing. Its metabolic products can promote vascularisation and fibroblast proliferation, as well as regulate collagen synthesis. Galli et al. [15] did not find that hyaluronic acid promotes wound healing after oral implant surgery, which may be related to the late assessment time (10 days post-surgery), the subjective scoring system, and the small sample size. In summary, whether hyaluronic acid can promote wound healing after implant surgery remains to be confirmed by further studies.
4 Application of hyaluronic acid in drug delivery systems
As a carrier, hyaluronic acid can deliver various drugs to specific pathological sites, enabling targeted drug delivery and slow release at the site of action, thereby significantly enhancing drug efficacy. In the field of dentistry, hyaluronic acid is often combined with BMP to form a composite, which is applied to the surface of implants to enhance early osseointegration and promote early stability of implants [17]; or it can be injected into the implant site after radiation therapy to slowly release BMP and exert its bone-inducing effects; additionally, hyaluronic acid can be combined with recombinant human BMP-2 and placed within the periosteum to induce osteogenesis, thereby improving the repair of bone defects. Due to its inherent fluidity and adhesive properties, hyaluronic acid not only induces bone formation but also serves as a biological coating material, making it an excellent carrier.
5 Application of hyaluronic acid in recurrent aphthous ulcers
Recurrent aphthous ulcers (RAU) are common lesions occurring on oral mucosa. Local treatment aims to reduce inflammation, relieve pain, prevent secondary infection, and promote ulcer healing. Nolan et al. [16] treated RAU with a 0.2% hyaluronic acid gel, applied 2–3 times daily, which immediately alleviated symptoms and promoted ulcer healing. Lee et al. [17] investigated the efficacy and safety of locally applying a 0.2% hyaluronic acid gel for RAU. Specifically, 33 patients with RAU were treated with 0.2% hyaluronic acid gel applied topically twice daily for two weeks, and their subjective and objective evaluation indicators were recorded.
The results showed that 75.8% of patients experienced improvement in pain visual analogue scale scores, 57.6% had a reduction in objective ulcer counts, 78.8% had a decrease in ulcer area, and all patients demonstrated significant improvement in inflammatory signs with no adverse reactions. Thus, topical application of 0.2% hyaluronic acid gel is safe and effective for the treatment of RAU. Hyaluronic acid may act as a barrier membrane to protect mucous membranes from oral environmental stimuli, while the improvement in inflammation is attributed to its anti-inflammatory and anti-edematous properties.
References
[1] Huang Sili, Guo Xueping, Yang Guilan, et al. Recent Advances in the Application of Hyaluronic Acid [J]. Food and Medicine, 2009, 11(1): 50-53.
[2] Long X, Chen G, Cheng AH, et al. A randomized con- trolled trial of superior and inferior temporomandibular joint space injection with hyaluronic acid in treatment of anterior disc displacement without reduction [J]. J Oral Maxillofac Surg, 2009, 67(2):357-361.
[3] Escoda-Francolí J, Vzquez-Delgado E, Gay-Escoda C.Scientific evidence on the usefulness of intraarticular hyaluronic acid injection in the management of temporo- mandibular dysfunction[J]. Med Oral Patol Oral Cir Bucal, 2010, 15(4):e644-e648.
[4] Li Chunjie, Zhang Yifan, Jia Yuanyuan, et al. A systematic review of a clinical randomised controlled trial on the treatment of temporomandibular joint dysfunction with sodium hyaluronate [J]. West China Journal of Stomatology, 2011, 29(5): 488-493.
[5] Liu Peicai, Wang Dong, Peng Cheng, et al. Effects of sodium hyaluronate on matrix metalloproteinases 2 and 3 in synovial fluid of patients with temporomandibular joint osteoarthritis [J]. Chinese Journal of Stomatological Research: Electronic Edition, 2011, 5(4): 356-360.
[6] Zhao Jigang, Peng Guoguang, Liang Jingzhang, et al. Clinical study on the prevention of postoperative complications of condylar fracture by joint lavage and sodium hyaluronate injection [J]. Journal of Modern Stomatology, 2011, 25(2): 105-107.
[7] Wu Yafei, Huang Jiao, Xu Yi, et al. The role of Gengigel gel in the treatment of plaque-induced gingivitis [J]. Journal of Practical Stomatology, 2005, 21(4): 540-542.
[8] Sukumar S, Drízhal I. Hyaluronic acid and periodontitis [J]. Acta Medica (Hradec Kralove), 2007, 50(4): 225-228.
[9] Xu Yi, Frentzen M, JervΦe-Storm P-M. The role of hyaluronic acid in the treatment of chronic periodontitis [J]. West China Journal of Stomatology, 2004, 22(1): 32-34.
[10] Fawzy El-Sayed KM, Dahaba MA, Aboul-Ela S, et al. Local application of hyaluronan gel in conjunction with periodontal surgery: A randomised controlled trial [J]. Clin Oral Investig, 2012, 16(4): 1229-1236.
[11] Zhang Li, Chen Gang, Ma Lian, et al. Clinical study on the treatment of peri-implant mucositis with sodium hyaluronate [J]. Chinese Journal of Oral Implantology, 2005, 10(1): 22-24.
[12] Mendes RM, Silva GA, Lima MF, et al. Sodium hyaluronate accelerates the healing process in tooth sockets of rats [J]. Archives of Oral Biology, 2008, 53(12): 1155-1162.
[13] Zeng Yunting, Tang Guohua. The effect of drugs on the healing of extraction sockets [J]. Oral Materials and Instruments, 2010, 19(2): 104-107.
[14] Lai, H. B., & Liu, Y. The role of hyaluronic acid gel in wound healing after implant surgery [J]. Guangdong Journal of Stomatology, 2008, 16 (Supplement): 637-638.
[15] Galli F, Zuffetti F, Capelli M, et al. Hyaluronic acid to improve healing of surgical incisions in the oral cavity: A pilot multicentre placebo-controlled randomised clinical trial [J]. Eur J Oral Implantol, 2008, 1(3): 199-206.
[16] Nolan A, Baillie C, Badminton J, et al. The efficacy of topical hyaluronic acid in the management of recurrent aphthous ulceration[J]. J Oral Pathol Med, 2006, 35(8): 461-465.
[17] Lee JH, Jung JY, Bang D. The efficacy of topical 0.2% hyaluronic acid gel on recurrent oral ulcers: Comparison between recurrent aphthous ulcers and the oral ulcers of Behçet's disease[J]. J Eur Acad Dermatol Venereol, 2008, 22(5): 590-595.


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese