Study on the Use of Hyaluronic Acid on Antimicrobial Agent
Infectious diseases caused by pathogenic bacteria (especially drug-resistant bacteria) are one of the greatest threats to global health [1]. With the widespread use of antimicrobial drugs, pathogenic bacteria are showing a trend of increasing resistance to antimicrobial drugs. The emergence of multi-drug resistant superbugs, the ‘ESKAPE’ bacteria [2] (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter Baumannii, Pseudomonas aeruginosa, and Enterobacter spp.), has caused great difficulties in clinical treatment and consumed a large amount of medical and health resources. In the face of the increasingly serious global problem of bacterial resistance, in addition to the rational control of the use of antimicrobial drugs, it is also urgent to actively search for new materials that resist bacterial resistance.
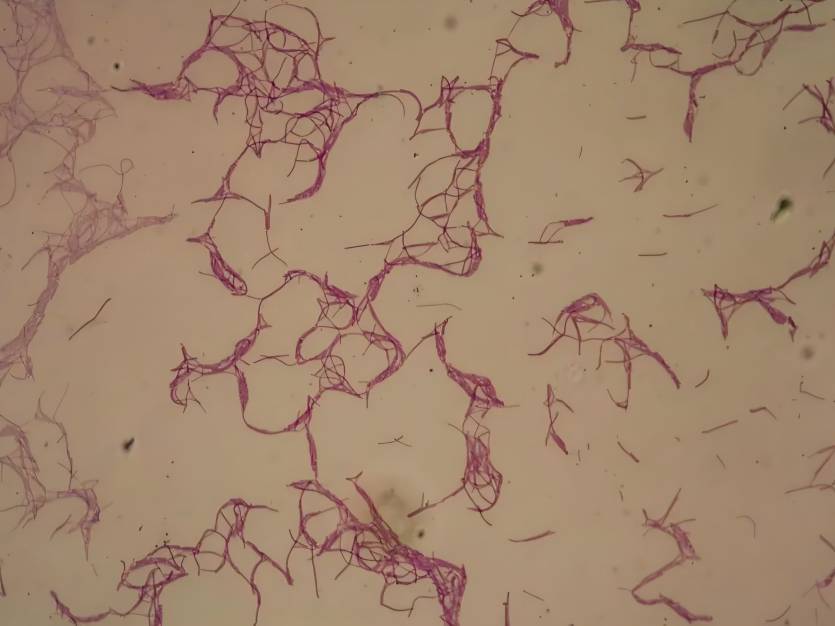
Hyaluronic acid, also known as sodium hyaluronate, is a high-molecular-weight acidic linear mucopolysaccharide widely distributed in the extracellular matrix of human connective tissue cells. It is composed of D-glucuronic acid and N-acetylglucosamine linked by β-1,4- and β-1,3-glycosidic bonds, with a molecular weight ranging from 1 to 10,000 kDa [3]. with multiple physiological functions such as maintaining cell structure and providing an energy source [4]. Due to its biocompatibility, non-immunogenicity and hydrophilic properties, hyaluronic acid has been widely used in the biomedical field in recent years: for example, to prevent adhesion during surgery [5], treat knee osteoarthritis [6], repair skin damage [7], and as artificial tears [8].
It is worth noting that the construction of new antimicrobial agent systems with the help of hyaluronic acid's anti-adhesion [9], receptor recognition [10], and easy structural modification [11] properties has become one of the current research hotspots for the development of new antimicrobial drugs at home and abroad. The molecular structure and properties of hyaluronic acid and its role in antimicrobial agents are shown in Figure 1. This article summarizes and discusses the application and development of hyaluronic acid in antimicrobial agents in recent years.
1 Antibacterial properties of hyaluronic acid
With the wide clinical application of hyaluronic acid, researchers have begun to pay attention to its effect on pathogenic bacteria. The earliest research by Tiunnikov's group [12] found that hyaluronic acid has obvious antiviral activity against herpes simplex virus type 2 (HSV-2), rubella virus, Newcastle disease virus and herpes simplex virus type 1 (HSV-1). Subsequently, Cermelli et al. [13] found that hyaluronic acid had strong antiviral activity against Coxsackievirus B5, mumps virus and influenza A H1N1 virus, and weaker effects against genital herpes virus HSV-1 and porcine parvovirus. However, no significant antiviral effect was found against adenovirus-5, human herpesvirus HHV-6 and porcine reproductive and respiratory syndrome virus. Meanwhile, the research group Ardizzoni et al. [14] also investigated in depth the effect of hyaluronic acid on bacteria including clinically relevant conditionally pathogenic bacteria, as well as fungal species. It was found that staphylococcus, enterococcus, proteus, Escherichia coli (ATCC 10536 and ATCC 25922), Pseudomonas aeruginosa, Candida albicans and Bacillus subtilis all showed hyaluronic acid dose-dependent growth inhibition. Streptococcus sanguinis was also inhibited at high hyaluronic acid concentrations, while Escherichia coli (ATCC 13768) and Candida albicans were not controlled at the highest concentration.
There are currently three main ways to study the antibacterial mechanism of hyaluronic acid.
1.1 Phagocytosis
CD44 is a transmembrane adhesion molecule whose main function is to bind and internalise hyaluronic acid. The entry of hyaluronic acid into the body and its specific binding to CD44 can lead to cytoskeleton restructuring, activation and increased bacterial phagocytosis by macrophages/monocytes, while further enhancing the anti-inflammatory effect [15]. However, the antibacterial properties of hyaluronic acid, which enhances bacterial phagocytosis, are limited by its concentration and molecular weight [16]. Some scholars [17] found that low molecular weight hyaluronic acid (<250 kDa) tends to increase the production of inflammatory mediators in macrophages; in contrast, high molecular weight hyaluronic acid (>800 kDa), which is mainly found in the extracellular matrix, promotes the production of anti-inflammatory mediators. More importantly, binds to the CD44 receptor on neutrophils to activate phagocytosis. It is the medium molecular weight hyaluronic acid (approx. 500 kDa) that is most effective in phagocytosis.
1.2 Anti-adhesive effect
Hyaluronic acid effectively reduces the adhesion of bacteria to cell and polymer substrates by interfering with the interaction of bacterial ligands and surface receptor sites and by forming a hydrated layer via the polysaccharide-water interaction, which shields the underlying substrate [18]. The anti-adhesive properties of hyaluronic acid can further prevent the formation of bacterial biofilms caused by bacterial adhesion and aggregation and the secretion of large amounts of polysaccharide proteins [19]. Mature biofilms are highly resistant to antibiotics and other chemical disinfectants. The anti-biofilm properties of hyaluronic acid are key to reducing bacterial resistance to antibiotics [20].

1.3 Reduce bacterial tissue permeability
Some studies have shown that pathogenic bacteria can produce a pathogenic bacterial spread factor-hyaluronidase-which catalyses the degradation of hyaluronic acid through the enzyme's β-elimination process. Hyaluronic acid is an important component of the extracellular matrix. Once degraded by bacterial lysozyme, it increases the tissue permeability of pathogenic bacteria, thereby promoting bacterial transmission and causing bacterial infections. However, excessive hyaluronic acid saturates the hyaluronidase of the bacteria, effectively preventing the bacteria from destroying the extracellular matrix, reducing the tissue permeability of the bacteria and reducing their vitality [21].
To date, there have been few reports of hyaluronic acid being used as an antibacterial agent alone. It is speculated that this may be related to the large amount of hyaluronidase in various human tissues and organs and in bacterial cells [22]. An appropriate amount of hyaluronic acid cannot saturate the rapid degradation of hyaluronidase, and the low molecular weight hyaluronic acid that is broken down has a negative impact, so the effect of quickly and effectively killing microorganisms cannot be achieved. Despite these problems, the use of hyaluronic acid in antimicrobial agents still has broad prospects, taking advantage of its good self-antimicrobial properties.
2 Hyaluronic acid-based antimicrobial agents
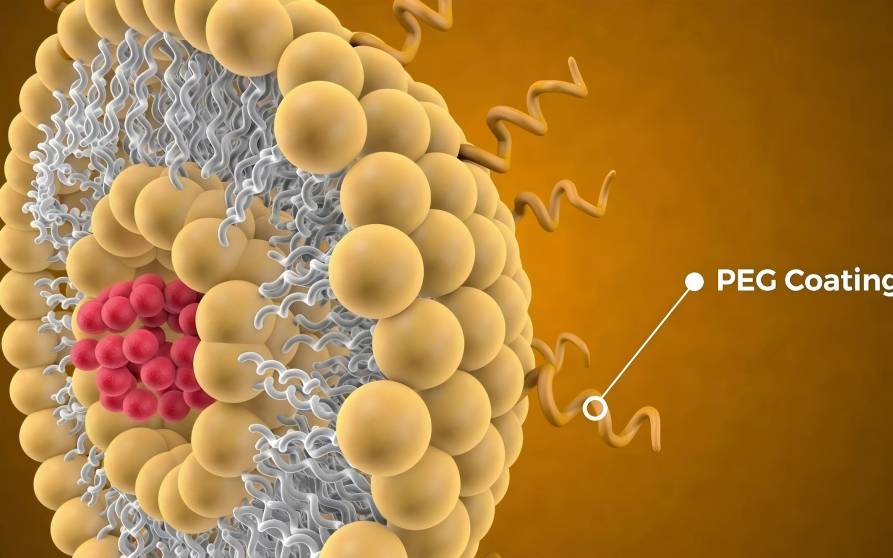
The use of hyaluronic acid in antimicrobial agents not only benefits from its biocompatible, non-immunogenic and hydrophilic biochemical properties, but also from its unique molecular structure. The presence of three functional groups-carboxyl, hydroxyl and acetamido-in the hyaluronic acid molecule makes it an ideal material for structural modification [23]. Hyaluronic acid is combined with antimicrobial drugs through physical and chemical actions to form various cross-linked gels[24], micelles[25], nanocremes[26], nanoparticles[27] and other antimicrobial agents that have also been developed and applied in the medical field. Among these antimicrobial agents, hyaluronic acid mainly plays three roles: targeted recognition, sustained-release matrix, and transport vector.
2.1 Hyaluronic acid-an antimicrobial targeting recognition molecule
2.1.1 Hyaluronic acid-CD44 receptor targeting host cells
During the attack of pathogenic bacteria, an inflammatory response often occurs as an adaptive defence response of the body. Using the two characteristics of high expression of CD44 on endothelial cells and mononuclear macrophages and the specific binding of hyaluronic acid to CD44 [28], hyaluronic acid can be used as a carrier for antimicrobial drugs, which is expected to achieve targeted drug delivery to the site of inflammation infected by pathogenic bacteria. In recent years, scientists have done a lot of exploration and experimentation with hyaluronic acid-CD44 targeted antimicrobial agents [29-31].
Lu et al. from Northwest A&F University [25] coupled the antimicrobial agent levofloxacin to hyaluronic acid via o-phenylenediamine to prepare nitric oxide ( NO-sensitive hyaluronic acid-based levofloxacin nanomicelles (HA-NO-LF) were prepared. HA-NO-LF can enter host cells through hyaluronic acid-CD44-mediated endocytosis. exposure to endogenous NO, and gradual drug release. It has a strong therapeutic effect on pulmonary infectious diseases. HA-NO-LF has a better in vivo bactericidal effect on Staphylococcus aureus than levofloxacin, which fully demonstrates the advantages of hyaluronic acid-based CD44 receptor recognition for targeted treatment of infectious diseases.
Arshad et al. [26] chemically bonded hyaluronic acid to the antibacterial drug ciprofloxacin to prepare a hyaluronic acid-functionalised nanoemulsion droplet drug delivery system. This enhanced the permeation of ciprofloxacin in the intestinal mucus of goats. The targeted treatment of intestinal infections caused by Salmonella was achieved by the specific uptake of hyaluronic acid by the CD44 receptor overexpressed on inflammatory intestinal cells. This nanoemulsion system not only enhances its antibacterial activity compared to ciprofloxacin, but also exhibits higher biocompatibility and better oral pharmacokinetics, further demonstrating the advantages of hyaluronic acid's good biocompatibility and targeted antibacterial properties.
Dubashynskaya et al. [32] prepared a hyaluronic acid-based polymyxin-loaded polymeric carrier, which with the aim of improving the drug delivery effect of colistin for the treatment of infections caused by multi-drug resistant Gram-negative bacteria. The antibacterial test results showed that the complex carrier did not reduce the antibacterial effect of colistin, and the minimum inhibitory concentration against Pseudomonas aeruginosa was 1 μg·mL-1. The results of pharmacokinetic studies showed that the hyaluronic acid-based colistin-loaded polymeric carrier could achieve slow release of colistin. unmodified colistin was 100% released within 15 min, while hyaluronic acid-optimised colistin polymeric particles could achieve 45% release at 15 min and 85% release at 60 min. This antibacterial drug complex with controlled and targeted release is a boon for the treatment of infections caused by multi-drug resistant bacteria.
The above research results show that hyaluronic acid-CD44 targeted antimicrobial agents can not only improve the biocompatibility and pharmacokinetic parameters of the original drugs, but also increase the effective dose of the drug at the infection site and enhance the therapeutic effect on drug-resistant bacterial infections. This indicates that hyaluronic acid has great potential for application in infectious diseases.
2.1.2 Hyaluronic acid-hyaluronidase targeting pathogenic bacteria
With the development of molecular biology technology, the presence of hyaluronidase has been found in a variety of pathogenic bacteria, including streptococci, staphylococci, enterococci, Clostridium, anaerobic bacilli, and streptomyces [33]. Some literature [34] has pointed out that the amount of hyaluronidase secreted by the bacteria reaches a maximum before the exponential growth period of the strain begins, which means that high levels of hyaluronidase can be considered an early sign of bacterial infection.
Hyaluronic acid loaded with antimicrobial agents is hydrolyzed by hyaluronidase released by pathogenic bacteria, and the antimicrobial drugs are released in a targeted manner to exert their efficacy [35]. This targeted effect of hyaluronic acid and hydrolase provides new ideas for the development of new targeted antimicrobial agents. For example, Liu Yuda et al. [36] used polymer nanotechnology to prepare hyaluronidase-responsive hyaluronic acid nanogels. Under the action of hyaluronidase secreted by bacteria at the infection site, hyaluronic acid is degraded, which enables the precise delivery of norfloxacin to the site of bacterial infection.

Yu Ningxiang et al. [37] reported a hyaluronic acid/silver nanoparticle/gentamicin nanocarrier triggered by hyaluronidase. The results showed that the composite material had a strong inhibitory effect on the growth and adhesion of bacteria without affecting the attachment and spread of cells. Most importantly, in vivo experimental results showed that the composite material could significantly inhibit the growth of Staphylococcus aureus in rat wounds and accelerate wound healing. Similarly, Ran et al. [38] developed a hyaluronidase-triggered photothermal platform based on hyaluronic acid-protected silver nanoparticles and graphene oxide for the treatment of bacterial infections. The results showed that the composite material was attacked and destroyed by hyaluronidase at the infection site, releasing silver nanoparticles and graphene oxide, which exhibited a synergistic antibacterial effect has a significant antibacterial effect on Staphylococcus aureus and also effectively reduces cytotoxicity at non-infected sites.
In summary, an antibacterial preparation based on hyaluronic acid-hyaluronidase is an antibacterial composite system that releases antibacterial drugs on demand and in situ, that is, it can achieve controlled drug release at the site of infection of pathogenic bacteria, which is of great significance for the treatment of drug-resistant bacterial infections.
2.2 Hyaluronic acid-wound site sustained-release matrix for antibacterial drugs
Severe body surface damage caused by surgery, trauma, burns or chronic diseases such as diabetes or peripheral vascular disease has become one of the most important clinical problems. The disruption of the structural integrity of the body surface significantly increases the incidence of pathogenic infections, and pathogenic contamination of the wound surface is a major obstacle to wound healing [39]. Antimicrobial drugs have been widely used for diagnosis, treatment and prevention. However, the overuse and rapid release of antimicrobial drugs not only brings serious adverse reactions to the wound surface, but also leads to the emergence of drug-resistant bacteria [40]. Hyaluronic acid has good water absorption, biocompatibility and inherent bioadhesiveness [41]. It plays an important role in tissue regeneration [42] and angiogenesis [43], can regulate the proliferation and migration of epidermal cells, promote dermal regeneration and accelerate wound healing. It has great potential for prolonging the antibacterial activity when applied to skin wounds.
Hyaluronic acid is used as a sustained-release matrix for the delivery of antimicrobial drugs, mostly in the form of wound dressings [44-45], with hydrogel dressings being the main type [46]. Zhu Jie et al. [47] used a composite hydrogel of aminoethyl methacrylate hyaluronic acid and methacrylate methoxypolyethylene glycol in combination with a nano-gel loaded with chlorhexidine diacetate to to construct a new composite hydrogel, and used a mouse model and agar plate diffusion test to evaluate its wound healing and antibacterial properties. The results showed that this hyaluronic acid-based hydrogel has cell compatibility, sustained antibacterial properties, hemostatic and wound healing abilities.
JON et al. [48] reported a novel wound dressing based on a mixed matrix of sodium alginate, hyaluronic acid and silver nanoparticles. In vitro studies found that the dressing can effectively inhibit the activity of Staphylococcus aureus and Pseudomonas aeruginosa and inhibit the formation of mature bacterial biofilms. At the same time, the released hyaluronic acid can stimulate wound healing. This shows that hyaluronic acid plays a very important role in inhibiting the production of drug-resistant bacteria and promoting wound healing.
To investigate the relationship between hyaluronic acid concentration and the effect of drug sustained release, Marinelli et al. [49] studied the effect of different ratios of hyaluronic acid in drug-loaded gels on antibacterial properties and viscoelastic properties. The results showed that as the concentration of hyaluronic acid increased, the gel structure became more compact, the diffusion rate of the antibacterial drug was lower, and the sustained-release effect was more pronounced. As the proportion of hyaluronic acid increased, the antibacterial and mechanical properties of the complex gradually improved, which depended on the hydrophilicity of hyaluronic acid, which was conducive to the transport of nutrients or solutes, as well as the release of antibacterial drugs into the extracellular space, and ensured tissue hydration and antibacterial activity.
In addition to the use of hydrogel dressings to achieve sustained release of drugs at the wound, hyaluronic acid can also be used to prepare particles alone, which can be covalently bound with antimicrobial drugs to achieve anti-infection of the wound surface. For example, Zhang et al. [50] prepared hyaluronic acid particles with adjustable antimicrobial drug loading by combining chemical bonding and physical adsorption. These hyaluronic acid particles can directly interact with the corneal anterior mucin layer, so that the drug-loaded particles can effectively adhere to ocular wounds, increasing the residence time of the drug in the postoperative wound, thereby achieving a long-term stable release of the antimicrobial drug.
In summary, the application of hyaluronic acid to wound dressings for the purpose of preventing infection helps to absorb wound exudates and maintain the mechanical integrity of the wound surface. It also helps to increase the retention time of antimicrobial drugs on the wound surface, reduce drug loss, lower the incidence of drug resistance and improve bioavailability.
2.3 Hyaluronic acid-a carrier for transporting antimicrobial drugs in the body
According to the way hyaluronic acid carries antimicrobial drugs, there are currently two main types of in vivo antimicrobial drug carriers based on hyaluronic acid. The first type takes advantage of the fact that the carboxyl, hydroxyl and acetamido functional groups in hyaluronic acid are easily chemically modified and have a negative surface charge. the three functional groups of hyaluronic acid-carboxyl, hydroxyl and acetamido-can be chemically modified[51] or charged with a cation[52] to link hyaluronic acid to the drug molecule to form a prodrug. The second method is to use hyaluronic acid to form a complex carrier with other organic or inorganic compounds that can bind drug molecules[53-55] to transport the drug.
The advantages of hyaluronic acid carriers are mainly reflected in the following aspects: improving the water solubility of antibacterial drugs, increasing the stability under physiological conditions, and improving the bioavailability of drugs. Sharma et al. [56] chemically bonded hyaluronic acid to curcumin, utilising the high hydrophilicity of hyaluronic acid, which improved the poor water solubility of curcumin and the limited efficacy of conventional antibacterial drug delivery. Gamarra et al. [52] coupled the brominated alkyltrimethylammonium quaternary phosphonium salt surfactant to hyaluronic acid to form an ionic complex with a comb-like stable structure, which exhibited good antibacterial properties. Liu et al. [54] introduced hyaluronic acid to improve the aggregation and poor water dispersibility of vancomycin-encapsulated organometallic frameworks (zeolite imidazolate framework, ZIF-8). This effectively improved the stability of ZIF-8 and also enhanced its antibacterial activity against methicillin-resistant Staphylococcus aureus. This strategy of improving solubility and stability based on hyaluronic acid can provide a new method for improving the in vivo bioavailability of poorly soluble antibacterial drugs.

It reduces drug cytotoxicity and improves biocompatibility. For example, Yuan et al. [53] used hyaluronic acid to covalently bind cationic conjugated oligomers (oligo-thiophene ethynylene, OTE) with antimicrobial activity to form nanoparticles with OTE ends encapsulated in the core. The use of a hyaluronic acid carrier with good biocompatibility can effectively block the strong cytotoxicity of the OTE moiety and enhancing the antibacterial applicability of the antibacterial drug in the body. Kłodzińska et al. [57] prepared a kind of octenyl succinic anhydride-modified low molecular weight hyaluronic acid (OSA-HA) nanogel as a transport carrier for azithromycin. Compared with unmodified azithromycin, OSA-HA can significantly reduce the cytotoxicity of azithromycin itself, increase its anti-Pseudomonas aeruginosa biofilm properties, and improve the treatment effect of infections.
It can reduce the damage caused by antimicrobial drugs and improve and control the drug loading. Intestinal probiotics are often used in the clinic as competitive inhibitors of pathogenic bacteria, but the oral administration of most probiotics often results in a significant loss of their vitality and biological activity due to the high acid and high bile salt environment in the gastrointestinal tract. Xiao Yao et al. [58] used a hyaluronic acid self-crosslinking hydrogel to encapsulate Lactobacillus rhamnosus. This hydrogel not only protects the probiotics from the erosion of gastrointestinal fluids, but also improves the activity of the probiotics in the gastrointestinal tract. It can also achieve the targeted release of probiotics in the intestine, enhancing the efficacy of salmonella enteritis. Other studies have found that by using a combination of chemical coupling and physical adsorption, ciprofloxacin can be encapsulated in transparent hyaluronic acid composite particles, which can increase the drug loading of ciprofloxacin by nearly 6.5 times. Bacteriostatic tests have shown that the composite has a tendency to gradually increase its bacteriostatic effect on Escherichia coli, Pseudomonas aeruginosa and Bacillus subtilis over time [59].
Increasing the local drug concentration reduces systemic adverse reactions. Due to the poor permeability of antimicrobial drugs across the cell membrane of eukaryotic cells, the active concentration in cells is limited. Treating intracellular infections usually involves increasing the efficacy by prolonging the duration of antimicrobial drug use and increasing the dose of the drug. However, these methods not only greatly increase the adverse reactions of antimicrobial drugs, but also lead to the generation of drug-resistant bacteria [60].
Wang Zhaojie et al. [61] loaded amikacin onto hyaluronic acid, which can be quickly delivered into cells via various carrier proteins on the cell membrane surface, such as CD44, to increase the intracellular drug concentration and achieve the goal of effectively eliminating intracellular bacteria. Qiu et al. [51] also used the receptor-mediated entry of hyaluronic acid into host cells to chemically couple hyaluronic acid with streptomycin. This combination can improve the intracellular bactericidal ability of VERO cells and RAW264.7 cells, and exhibits less nephrotoxicity. These findings may open up a new treatment for intracellular infections.
3 Conclusion and outlook
With the wide application of hyaluronic acid in biomedicine, hyaluronic acid is also gradually showing unique advantages in antibacterial applications and has broad application prospects. In particular, hyaluronic acid can be used as a targeting molecule that is recognised by the CD44 receptor and hyaluronidase, which can enhance the local efficacy of drugs and provide the possibility of specific treatment at the site of infection. Hyaluronic acid can also be used as a sustained-release matrix and drug carrier, which is beneficial for prolonging the action time of antimicrobial drugs, controlling the use of antimicrobial drugs, reducing drug cytotoxicity, and improving drug compliance. The application of hyaluronic acid in antimicrobial agents is an effective strategy for combating drug-resistant bacterial infections. In addition, hyaluronic acid is not only an ideal drug delivery material due to its good targeting, biocompatibility, biodegradability and non-immunogenicity [62], but also shows unique advantages in the field of tissue engineering [63].
Hyaluronic acid hydrogels used as wound dressings for traumatic injuries can, on the one hand, help with the local release of antimicrobial drugs and, on the other hand, physically block the effects of external pathogens. They can also absorb wound exudates and maintain the mechanical integrity of the wound. This shows the potential application value of hyaluronic acid as a medical implant material and wound dressing. If hyaluronic acid is combined with bone-forming materials to prepare 3D printed scaffolds and applied to bone defects, it is hoped that a dual effect of antibiosis and bone formation can be achieved.
However, there are still some drawbacks to using hyaluronic acid in antimicrobial agents, such as the presence of a large number of hyaluronidases in various tissues and organs of the human body. These hyaluronidases cause hyaluronic acid to degrade rapidly in the body. Current research is mostly based on chemical modification to enhance the in vivo circulation time of hyaluronic acid. However, the chemical coupling process is complicated, and the product is difficult to purify, which poses difficulties for the further antimicrobial application of hyaluronic acid. Despite the many problems and challenges, hyaluronic acid is still a very promising antimicrobial material. It is believed that in subsequent research, the combination of developments in multiple disciplines such as materials science, pharmacology, physiology and tissue engineering will gradually improve and promote the better application of hyaluronic acid in the field of medical antimicrobial.
Reference
[1]QIAO M, YING G G, SINGER A C, et al. Review of antibiotic resistance in China and its environment[J]. Environ Int, 2018(110): 160-172.
[2]MA Y X, WANG C Y, LI Y Y, et al. Considerations and caveats in combating ESKAPE pathogens against nosocomial infections[J]. Adv Sci (Weinh), 2019, 7(1): 1901872. Doi: 10.1002/advs.201901872.
[3]ZHANG X D, WEI D Y, XU Y, et al. Hyaluronic acid in ocular drug delivery[J]. Carbohydr Polym, 2021(264): 118006. Doi: 10.1016/j.carbpol.2021.118006.
[4]LEE Y, SUGIHARA K, GILLILLAND M G 3rd, et al. Hyaluronic acid-bilirubin nanomedicine for targeted modulation of dysregulated intestinal barrier, microbiome and immune responses in colitis[J].Nat Mater,2020,19(1): 118-126.
[5]KIM S J, SHIN J M, LEE E J, et al. Efficacy of hyaluronic acid and hydroxyethyl starch in preventing adhesion following endoscopic sinus surgery[J]. Eur Arch Otorhinolaryngol, 2017, 274(10): 3643-3649.
[6]MIGLIORE A, BLICHARSKI T, PLEBANSKI R, et al. Knee osteoarthritis pain management with an innovative high and low molecular weight hyaluronic acid formulation (HA-HL): A randomized clinical trial[J].Rheumatol Ther, 2021, 8(4): 1617-1636.
[7]SEGRETO F, CAROTTI S, MARANGI G F, et al. The use of acellular porcine dermis, hyaluronic acid and polynucleotides in the treatment of cutaneous ulcers: Single blind randomised clinical trial[J]. Int Wound J, 2020, 17(6): 1702-1708.
[8]MOHAMMADPOUR M,KHORRAMI-NEJADM, SHAKOOR D. Role of artificial tears with and without hyaluronic acid in controlling ocular discomfort following PRK: A randomized clinical trial[J]. Int J Ophthalmol, 2021, 14(8): 1225-1230.
[9]MA W M, HUANG N, XIONG K Q. Construction of surface with anticoagulant and antibacterial functions via a covalent immobilization of hyaluronic acid with high density[J]. Mater Rep, 2020(8): 165-171.
[10]DONG Q B. Construction of an injectable and antibacterial hyaluronic acid hydrogel based on hybrid crosslinking strategy and its prevention of CIED pocket infection[D]. Nanchang:Nanchang University, 2021.
[11]DONG Y Q, LI L L, ZHU X R, et al. Preparation and roles of sliver-loaded viscous hydrogel in healing of full-thickness skin defect wounds with bacterial colonization in mice[J]. Chin J Burns, 2021, 37(11): 1036-1047.
[12]TIUNNIKOV G I, KOSTINA G A, RADAEVA I F, et al. Effects of hyaluronic acid preparation on the development of herpetic infection in cell culture[J]. Vopr Virusol, 2002, 47(1): 37-39.
[13]CERMELLI C, CUOGHI A, SCURI M, et al. In vitro evaluation of antiviral and virucidal activity of a high molecular weight hyaluronic acid[J]. Virol J, 2011(8): 141. Doi: 10.1186/1743-422X-8-141
[14]ARDIZZONI A, NEGLIA R G, BASCHIERI M C, et al. Influence of hyaluronic acid on bacterial and fungal species, including clinically relevant opportunistic pathogens[J]. J Mater Sci Mater Med, 2011, 22(10): 2329-2338.
[15]ZHOU L, HAO Q, SUGITA S, et al. Role of CD44 in increasing the potency of mesenchymal stem cell extracellular vesicles by hyaluronic acid in severe pneumonia[J]. Stem Cell Res Ther, 2021, 12(1): 293. Doi: 10.1186/s13287-021-02329-2.
[16]LEBAUDY E, FOURNEL S, LAVALLE P, et al. Recent advances in antiinflammatory material design[J]. Adv Healthc Mater, 2021, 10(1): e2001373. Doi: 10.1002/adhm.202001373.
[17]LEE J H, LIU A, PARK J H, et al. Therapeutic effects of hyaluronic acid in peritonitis-induced Sepsis in mice[J]. Shock, 2020, 54(4): 488-497.
[18]LARRAÑETA E, HENRY M, IRWIN N J, et al. Synthesis and characterization of hyaluronic acid hydrogels crosslinked using a solvent-free process for potential biomedical applications[J]. Carbohydr Polym, 2018(181): 1194-1205.
[19]ROMANÒ C L, DE VECCHI E, BORTOLIN M, et al. Hyaluronic acid and its composites as a local antimicrobial/antiadhesive barrier[J]. J Bone Jt Infect, 2017, 2(1): 63-72.
[20]MARCUZZO A V, TOFANELLI M, BOSCOLO NATA F, et al. Hyaluronate effect on bacterial biofilm in ENT district infections: A review[J]. APMIS, 2017, 125(9): 763-772.
[21]CARLSON G A, DRAGOO J L, SAMIMI B, et al. Bacteriostatic properties of biomatrices against common orthopaedic pathogens[J]. Biochem Biophys Res Commun, 2004, 321(2): 472-478.
[22]LEI X, ZHANG R, HUANG Z X, et al. Research progress of hyaluronidases[J]. J Microbiol China, 2021, 48(3): 882-895.
[23]TIWARI S, BAHADUR P. Modified hyaluronic acid based materials for biomedical applications[J]. Int J Biol Macromol, 2019(121): 556-571.
[24]MAKVANDI P, ASHRAFIZADEH M, GHOMI M, et al. Injectable hyaluronic acid-based antibacterial hydrogel adorned with biogenically synthesized AgNPs-decorated multi-walled carbon nanotubes[J]. Prog Biomater, 2021, 10(1): 77-89.
[25]LU C B, XIAO Y, LIU Y Y, et al. Hyaluronic acid-based levofloxacin nanomicelles for nitric oxide-triggered drug delivery to treat bacterial infections[J]. Carbohydr Polym, 2020(229): 115479.[26]ARSHAD R, TABISH T A, KIANI M H, et al. A hyaluronic acid functionalized self-nano-emulsifying drug delivery system (SNEDDS) for enhancement in ciprofloxacin targeted delivery against intracellular infection[J]. Nanomaterials(Basel), 2021, 11(5): 1086. Doi: 10.3390/nano11051086.
[27]JIANG T, XIE Z, WU F, et al. Hyaluronic acid nanoparticle composite films confer favorable time-dependent biofunctions for vascular wound healing[J]. ACS Biomater Sci Eng, 2019, 5(4): 1833-1848.
[28] Fu Qiang, Wang Aifu, Chen Yanfeng, et al. Research progress of the CD44 gene in the process of bacterial infection [J]. China Animal Husbandry and Breeding, 2016, 12(6): 32-33.
[29]MELO C M, CARDOSO J F, PERASSOLI F B, et al. Amphotericin B-loaded Eudragit RL100 nanoparticles coated with hyaluronic acid for the treatment of vulvovaginal candidiasis[J]. Carbohydr Polym, 2020(230): 115608. Doi: 10.1016/j.carbpol.2019.115608.
[30]LI Y J, GAO Z G, ZHANG Y, et al. MOF-shielded and glucose-responsive ultrasmall silver nano-factory for highly-efficient anticancer and antibacterial therapy[J]. Chem Eng J, 2021(416): 127610. Doi: doi.org/10.1016/j.cej.2020. 127610.
[31]JORDAN A R, RACINE R R, HENNIG M J P, et al. The role of CD44 in disease pathophysiology and targeted treatment[J]. Front Immunol, 2015(6): 182. Doi: 10.3389/fimmu.2015. 00182.
[32]DUBASHYNSKAYA N V, RAIK S V, DUBROVSKII Y A, et al. Hyaluronan/colistin polyelectrolyte complexes: Promising antiinfective drug delivery systems[J]. Int J Biol Macromol, 2021(187): 157-165.
[33]LI M, LIU J J, SU J W, et al. Research and development of hyaluronidase[J]. Food Drug, 2019(4): 336-336, I0004.
[34]TÜCKING K S, GRÜTZNER V, UNGER R E, et al. Dual enzyme-responsive capsules of hyaluronic acid-block- poly(lactic acid) for sensing bacterial enzymes[J]. Macromol Rapid Commun, 2015, 36(13): 1248-1254.
[35]AYAZ P, XU B J, ZHANG X S, et al. A pH and hyaluronidase dual-responsive multilayer-based drug delivery system for resisting bacterial infection[J]. Appl Surf Sci, 2020(527): 146806. Doi: 10.1016/j.apsusc.2020.146806
[36]LIU Y D, CHEN D M, ZHANG A X, et al. Composite inclusion complexes containing hyaluronic acid/chitosan nanosystems for dual responsive enrofloxacin release[J]. Carbohydr Polym,2021(252): 117162. Doi: 10.1016/j.carbpol.2020.117162.
[37]YU N X, WANG X Y, QIU L, et al. Bacteria-triggered hyaluronan/AgNPs/gentamicin nanocarrier for synergistic bacteria disinfection and wound healing application[J]. Chem Eng J, 2020(380): 122582.
[38]RAN X, DU Y, WANG Z Z, et al. Hyaluronic acid-templated Ag nanoparticles/graphene oxide composites for synergistic therapy of bacteria infection[J]. ACS Appl Mater Interfaces, 2017, 9(23): 19717-19724.
[39]YANG Y, DONG Z G, LI M, et al. Graphene oxide/copper nanoderivatives-modified chitosan/hyaluronic acid dressings for facilitating wound healing in infected full-thickness skin defects[J]. Int J Nanomedicine, 2020(15): 8231-8247.
[40]JON A D O, JOSÉ M A, VIRGINIA S M, et al. Biocompatible hyaluronic acid-divinyl sulfone injectable hydrogels for sustained drug release with enhanced antibacterial properties against Staphylococcus aureus[J]. Mat Sci Eng C, 2021(125): 112102.
[41]WANG J. Prepared hydrogel dressing based on hyaluronic acid for combining with cell sheet and anti-bacteria[D]. Beijing: Beijing University of Chemical Technology, 2020.
[42]ZHAI P S, PENG X X, LI B Q, et al. The application of hyaluronic acid in bone regeneration[J]. Int J Biol Macromol, 2020(151): 1224-1239.
[43]YANG L L, ZHANG L T, HU J, et al. Promote anti- inflammatory and angiogenesis using a hyaluronic acid-based hydrogel with miRNA-laden nanoparticles for chronic diabetic wound treatment[J]. Int J Biol Macromol, 2021(166): 166-178.
[44]GRAÇA M F P, MIGUEL S P, CABRAL C S D, et al. Hyaluronic acid-Based wound dressings: A review[J]. Carbohydr Polym, 2020(241): 116364. Doi: 10.1016/j.carbpol. 2020.116364.
[45]TU Y Y, LI L H, ZHAO X Y, et al. Fermentation production of microbial polysaccharides and it’s application in wound dressings[J]. Chin J Mod Appl Pharm, 2021(17): 2185-2192.
[46]CORTES H, CABALLERO-FLORÁN I H, MENDOZA- MUÑOZ N, et al. Hyaluronic acid in wound dressings[J]. Cell Mol Biol: Noisy-Le-Grand, 2020, 66(4): 191-198.
[47]ZHU J, LI F X, WANG X L, et al. Hyaluronic acid and polyethylene glycol hybrid hydrogel encapsulating nanogel with hemostasis and sustainable antibacterial property for wound healing[J]. ACS Appl Mater Interfaces, 2018, 10(16): 13304-13316.
[48]TARUSHA L, PAOLETTI S, TRAVAN A, et al. Alginate membranes loaded with hyaluronic acid and silver nanoparticles to foster tissue healing and to control bacterial contamination of non-healing wounds[J]. J Mater Sci Mater Med, 2018, 29(3): 22.
[49]MARINELLI L,CACCIATORE I,EUSEPI P, et al. Viscoelastic behaviour of hyaluronic acid formulations containing carvacrol prodrugs with antibacterial properties[J]. Int J Pharm, 2020(582): 119306. Doi: 10.1016/j.ijpharm.2020. 119306.
[50]ZHANG Z, SUNER S S, BLAKE D A, et al. Antimicrobial activity and biocompatibility of slow-release hyaluronic acid-antibiotic conjugated particles[J]. Int J Pharm, 2020(576): 119024. Doi: 10.1016/j.ijpharm.2020.119024.
[51]QIU Y H, HOU Y L, SUN F F, et al. Hyaluronic acid conjugation facilitates clearance of intracellular bacterial infections by streptomycin with neglectable nephrotoxicity[J]. Glycobiology, 2017, 27(9): 861-867.
[52]GAMARRA A, FORÉS E, MORATÓ J, et al. Amphiphilic ionic complexes of hyaluronic acid with organophosphonium compounds and their antimicrobial activity[J]. Int J Biol Macromol, 2018, 118(Pt B): 2021-2031.
[53]YUAN Q, ZHAO Y T, ZHANG Z Q, et al. On-demand antimicrobial agent release from functionalized conjugated oligomer-hyaluronic acid nanoparticles for tackling antimicrobial resistance[J]. ACS Appl Mater Interfaces, 2021, 13(1): 257-265.
[54]LIU Y Y, LI Z H, ZOU S Y, et al. Hyaluronic acid-coated ZIF-8 for the treatment of pneumonia caused by methicillin- resistant Staphylococcus aureus[J].Int J Biol Macromol, 2020(155): 103-109.
[55]YANG J, ZHAO Y D, CAO J, et al. Hyaluronic acid and antimicrobial peptide-modified gold/silver hybrid nanocages to combat bacterial multidrug resistance[J]. Int J Pharm, 2020(586): 119505. Doi: 10.1016/j.ijpharm.2020.119505.
[56]SHARMA M, SAHU K, SINGH S P, et al. Wound healing activity of curcumin conjugated to hyaluronic acid: In vitro and in vivo evaluation[J]. Artif Cells Nanomed Biotechnol, 2018, 46(5): 1009-1017.
[57]KŁODZIŃSKA S N, WAN F, JUMAA H, et al. Utilizing nanoparticles for improving anti-biofilm effects of azithromycin: A head-to-head comparison of modified hyaluronic acid nanogels and coated poly(lactic-co-glycolic acid) nanoparticles[J]. J Colloid Interface Sci, 2019, 555: 595-606.
[58]XIAO Y, LU C B, LIU Y Y, et al. Encapsulation of Lactobacillus rhamnosus in hyaluronic acid-based hydrogel for pathogen-targeted delivery to ameliorate enteritis[J]. ACS Appl Mater Interfaces, 2020, 12(33): 36967-36977.
[59]SAHINER N, SUNER S S, AYYALA R S. Preparation of hyaluronic acid and copolymeric hyaluronic acid: Sucrose particles as tunable antibiotic carriers[J]. J Polym Res, 2020, 27(7): 1-12.
[60]LIU C X. Challenges and thinking of current antibiotic development[J]. Chin J Antibiot, 2017, 42(1): 1-12.
[61]WANG Z J, QIU Y H, HOU C Y, et al. Synthesis of hyaluronan-amikacin conjugate and its bactericidal activity against intracellular bacteria in vitro and in vivo[J]. Carbohydr Polym, 2018(181): 132-140.
[62]CHEN F, YANG Y, ZHANG L, et al. Research progress of hyaluronic acid-based nanodrug delivery systems in targeted cancer therapy[J]. Chin J Mod Appl Pharm, 2019(13): 1704-1710.
[63]LIU H, LIU A F, ZHANG Y, et al. Advantages and application strategies of hyaluronic acid scaffold in cartilage repair engineering[J]. Chin J Tiss Eng Res, 2022, 26(34): 5518-5524.


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese







