Study on Coenzyme Q10 Used for Osteoporosis Treatment
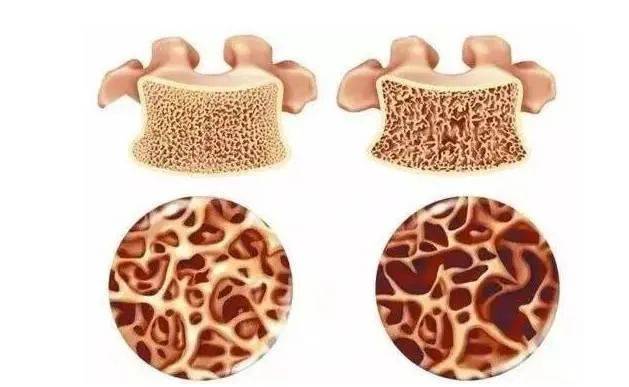
Osteoporosis (OP) occurs due to an imbalance between osteoblast differentiation and osteoclast resorption. It is characterized by a decrease in bone mass, deterioration of bone microstructure, high fracture risk, and late complications associated with severe morbidity and mortality. It is common in postmenopausal women and elderly men [1].
Coenzyme Q10 (CoQ10), or ubiquinone, consists of a benzoquinone ring with a redox-active center and a long polyisoprene lipid chain [2]. Coenzyme Q10 is derived from both endogenous synthesis and exogenous intake. In the human body, coenzyme Q10 is synthesized from tyrosine or phenylalanine to form the benzoquinone structure, and the polyisoprene side chain is synthesized from acetyl coenzyme A (CoA) via the methyl valerate pathway. and then the coenzyme Q10 is formed by further modification and condensation of the quinone ring structure by methods such as hydroxylation, methylation, and decarboxylation [3]; while external intake mainly comes from animal protein, vegetables, fruits, and cereals [4].

The conventional treatment of osteoporosis mainly focuses on drug therapy, and a large number of experiments have shown that long-term use of osteoporosis drugs can cause serious adverse reactions. Recent studies have shown that coenzyme Q10 can regulate bone metabolism and reduce the occurrence of osteoporosis. Therefore, this article provides a new direction for the prevention and treatment of osteoporosis by discussing the conventional treatment of osteoporosis, the mechanism, application, and safety of coenzyme Q10 in affecting bone metabolism.
1. Conventional Treatment of Osteoporosis
The current conventional treatment of osteoporosis is drug therapy, which is divided into two main categories: anti-bone resorption drugs and bone formation-promoting drugs.
1.1 Anti-bone Resorption Drugs
Anti-bone resorption drugs prevent bone loss by inhibiting the activation and function of osteoclasts. Representative drugs include bisphosphonates (BPs), denosumab, selective estrogen receptor modulators (SERMs), and calcitonin. Bisphosphonates include alendronate, risedronate, ibandronate and zoledronic acid, which inhibit bone resorption by binding to hydroxyapatite on the bone surface. Denosumab is a human recombinant monoclonal antibody that blocks the binding of receptor activator of nuclear factor-κB ligand (RANKL) to osteoclast cells [5] and inhibits osteoclast activity.
Selective estrogen receptor modulators exert their effect by selectively binding to estrogen receptors. receptor activator of nuclear factor-κB Ligand (RANKL) from binding to osteoclast cells [5], inhibiting osteoclast activity; selective estrogen receptor modulators exert an oestrogen-like effect by selectively binding to oestrogen receptors, reducing the production and activity of osteoclast cells [6]; calcitonin inhibits bone resorption by inhibiting the mechanism of calcium outflow from the bone. Anti-bone resorption drugs mostly have adverse reactions, especially in patients with osteoporosis who are treated for increased bone resorption caused by bone tumors, combined with diabetes, immunosuppression, steroids, smoking, and alcohol intake, with jaw necrosis and atypical fractures being common [7].
1.2 Osteogenic Drugs
Osteogenic drugs increase bone formation by promoting the differentiation of osteoblasts. A representative drug is a teriparatide. Teriparatide is recombinant human parathyroid hormone 1-34 (recombinant human parathyroid hormone 1-34, RHPTH 1-34), and the N-terminal amino acid sequence of teriparatide binds to osteoblast, mesenchymal cell, and type I parathyroid hormone receptor on the surface of the renal tubular basement membrane [8], exerting a bone-forming effect, and is commonly used in postmenopausal women with osteoporosis and a high risk of fracture. The disadvantages of teriparatide are its high price, serious adverse reactions, and the need for injection.
In summary, the disadvantage of osteoporosis drug therapy is that long-term administration can cause serious adverse reactions. Therefore, it is necessary to study safe and effective osteoporosis drugs.
2.Mechanism of Coenzyme Q10 Affecting Bone Metabolism
Coenzyme Q10 has many physiological functions, such as anti-oxidation, anti-inflammation, anti-apoptosis, scavenging free radicals and membrane stabilizing effects, but it mainly exerts anti-oxidation and anti-apoptosis effects in bone metabolism. Current research shows that coenzyme Q10 prevents bone loss by promoting osteoblast bone formation, inhibiting osteoclast bone resorption, and inhibiting oxidative stress and cellular aging.
2.1The Effect of Coenzyme Q10 on Osteoblasts and Osteoclasts
Osteoblasts originate from multipotent mesenchymal stem cells in the bone marrow and are the main functional cells responsible for bone formation. They are responsible for the synthesis, secretion, and mineralization of bone matrix. Osteoclasts originate from the multinucleated cells of the mononuclear-macrophage lineage hematopoietic progenitor cells and are the main functional cells responsible for bone resorption. They are responsible for bone development, growth, repair, and reconstruction. Studies have shown that coenzyme Q10 can promote bone formation.

Zheng et al. [9] used cell culture and a rat osteoporosis model to study bone marrow mesenchymal stem cells extracted from experimental rats and confirmed that CoQ10 can promote the proliferation of bone marrow mesenchymal stem cells and promote osteogenic differentiation in a dose-dependent manner [10]. In Wu et al.'s [11] study, antioxidant CoQ10 was injected into orchiectomy (ORX) mice were injected with the antioxidant CoQ10 for 40 weeks, and the results showed that CoQ10 effectively prevented ORX-induced bone loss by resisting oxidative stress. The antioxidant CoQ10 played a preventive and protective role in ORX-induced osteoporosis by promoting osteoblast bone formation, inhibiting osteoclast bone resorption and oxidative stress, and preventing cell senescence.
2.2 Coenzyme Q10 Reduces Oxidative Stress
Oxidative stress occurs when there is an increase in the formation of reactive oxygen species (ROS) a decrease in antioxidant activity, or both, in biological systems [12]. Excessive reactive oxygen species can inhibit the differentiation and proliferation of osteoblasts, promote the differentiation of osteoclasts, and ultimately lead to more bone resorption [13-14]. Dietary supplementation with antioxidants is an effective way to improve the damage caused by excessive reactive oxygen species [15].
Coenzyme Q10 is a natural antioxidant that has antioxidant and free radical scavenging effects, inhibits and reduces oxidative stress, and thus prevents osteoporosis. Zhang et al. [16] established a rat spinal cord injury (SCI) model and administered CoQ10 (10 mg/kg, gavage) daily for 12 h for more than 10 days. The results showed that after CoQ10 treatment, the rate of decrease in bone mineral density and bone mineral content in SCI rats was slowed; the level of malondialdehyde in the bone decreased, the level of superoxide dismutase increased, and the oxidative damage caused by the injury was alleviated; and the level of inflammatory cytokines was significantly reduced. This suggests that CoQ10 treatment can effectively reduce the occurrence of spinal cord injury-induced osteoporosis.
2.3 Coenzyme Q10 Inhibits the Effects of Cellular Senescence
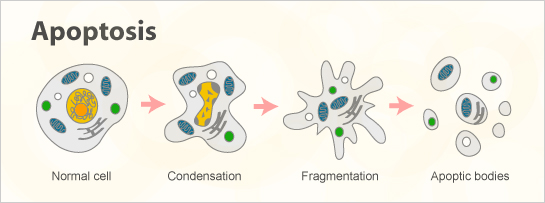
Cellular senescence is a state of cell cycle arrest that inhibits apoptosis and secretes multiple bioactive factors (senescence-associated secretory phenotype – SASP), which play physiological roles in embryonic development and the healing process [17]. Increased ROS is an important factor in the age-related changes of all tissues, including bone [18].
Some clinical and experimental data suggest that oxidative stress can lead to bone senescence. Oxidative stress in normal cells can lead to cellular senescence, and coenzyme Q10 has an antioxidant effect that can counteract cellular oxidative stress. Li et al. [19] established a spinal cord injury model to evaluate whether coenzyme Q10 can reduce oxidative stress and prevent apoptosis of bone marrow mesenchymal stem cells. The results showed that CoQ1 0 treatment significantly reduced the expression of the apoptotic proteins bax and caspase-3, while increasing the expression of the anti-apoptotic protein bcl-2 and antioxidant products, indicating that coenzyme Q10 has anti-apoptotic and antioxidant effects, can fight cell apoptosis, and thus prevent bone loss.
Zhang et al. [20] divided bone marrow mesenchymal stem cells into a control group, a D-galactose treatment group with different concentration gradients, and a CoQ10 treatment group with different concentrations to evaluate the effect of coenzyme Q10 on stem cell apoptosis. The results showed that Co Q10 significantly reduced the GAL-positive cells and the expression of p53, p21 and p16 in D-galactose-treated bone marrow mesenchymal stem cells, indicating that CoQ10 inhibits the aging of bone marrow mesenchymal stem cells by inhibiting the production of ROS.
3.Application of Coenzyme Q10 in the Treatment of Osteoporosis
Wang Kexin et al. [21] randomly divided 40 male mice into a normal control group, a D-galactose model group, a calcitriol group, and a coenzyme Q10 group, which were continuously administered for 12 weeks. At the end of the experiment, the femurs of the mice were used for micro-CT and bone biomechanical testing, and the gastrocnemius was examined by ultramicroscopic transmission electron microscopy.
The results showed that compared with the normal control group, the maximum load and stiffness coefficient of the femur in the model group were significantly reduced; the micro-CT parameters connectivity density (Conn. D) and bone mineral destiny (BMD) were significantly reduced, and trabecular separation (Tb. Sp) was significantly increased. Compared with the model group, the coenzyme Q10 group had a significantly higher maximum femur load, Conn. D., BMD, and trabecular thickness (Tb. Th), while the structure model index (SMI) and Tb. Sp decreased significantly.
In a study evaluating dietary fat unsaturation and coenzyme Q10 supplementation on bone health [22], 48 male rats were randomly divided into four groups: olive oil group, sunflower oil group, olive oil + coenzyme Q10 group, and sunflower oil + coenzyme Q10 group. Bone mineral density of the rats' femurs was measured, and the results showed that coenzyme Q10 can prevent bone mineral density loss.
In another experiment on the prevention of hormonal femoral head necrosis by coenzyme Q10 [23], 20 rats were divided into a control group and a coenzyme Q10 group, and bone necrosis was evaluated. The results showed that the coenzyme Q 10 group blood glutathione (GSH) and malondialdehyde (MDA) content changes were not significant, histological changes and the incidence of early osteonecrosis were lower than in the control group, and coenzyme Q10 has a protective effect on bone. The above confirms that coenzyme Q10 has a protective effect on bone, providing a scientific basis for the treatment of osteoporosis.
4.Safety of Coenzyme Q10
Coenzyme Q10 is now widely used in the pharmaceutical, food, and cosmetics industries. As research into coenzyme Q10 continues, its safety is also being investigated. Current research shows that coenzyme Q10 is highly safe, with good tolerance and few adverse reactions.
In animal experiments, Hong Yan et al. [24] conducted an Ames test on 50 mice, and the results showed that coenzyme Q10 does not have a mutagenic effect on genes. Wu Keqin et al. [25] conducted a 30-day gavage toxicity experiment, and the results showed that the rats did not have obvious abnormal activity or symptoms of poisoning.
Honda et al. [26] conducted a subchronic toxicology study of coenzyme Q10, giving rats daily doses of 300, 600, and 1,200 mg/kg for 13 weeks. The results showed that none of the groups showed signs of death or poisoning. In clinical studies, McGarry et al. [27] conducted a randomized double-blind trial in which subjects were given 2,400 mg of CoQ10 per day. The results showed that CoQ10 was well tolerated by the subjects and no serious adverse reactions occurred. In a clinical trial on progressive supranuclear palsy [28], 61 participants were given CoQ10 (2400 mg/d) or a placebo for 12 months, and their daily living abilities and mental states were assessed. The results showed that there was no significant difference between the CoQ10 group and the placebo group in the first or second outcome measurement, and the tolerance was very good.
5.Summary and Outlook
In summary, there are currently relatively few animal experiments and clinical studies on the use of coenzyme Q10 to treat osteoporosis. Large-scale animal experiments and clinical trials are therefore the focus for the next step. Coenzyme Q10 mainly plays a role in the prevention and adjuvant treatment of osteoporosis It is believed that with further basic and clinical research, coenzyme Q10 may become a new drug for the prevention and treatment of osteoporosis.
References:
[1] Vidal M,Thibodaux RJ,Neira LFV,et al. Osteoporosis:a clinical and pharmacological update [J]. Clin Rheumatol,2019,38(2):385-395.
[2] Díaz-Casado ME,Quiles JL,Barriocanal-Casado E,et al. The Paradox of Coenzyme Q(10)in Aging [J]. Nutrients,2019,11(9):2221.
[3] Hargreaves IP. Ubiquinone:cholesterol's reclusive cousin [J]. Ann Clin Biochem,2003,40(Pt 3):207-218.
[4] Gutierrez-Mariscal FM,Yubero-Serrano EM,Villalba JM,et al. Coenzyme Q(10):From bench to clinic in aging diseases,a translational review [J]. Crit Rev Food Sci Nutr,2019,59(14):2240-2257.
[5] Pang KL,Low NY,Chin KY. A Review on the Role of Denosumab in Fracture Prevention [J]. Drug Des Devel Ther,2020,14:4029-4051.
[6] Du Yanping, Cheng Qun. Mechanism and strategy of sequential treatment with parathyroid hormone analogues and bisphosphonates for osteoporosis [J]. Theoretical and Practical Diagnostics, 2020, 19(3): 219-224.
[7] Compston J,Cooper A,Cooper C,et al. UK clinical guideline for the prevention and treatment of osteoporosis [J]. ArchOsteoporos,2017,12(1):43.
[8] Dobnig H. A review of teriparatide and its clinical efficacy in the treatment of osteoporosis [J]. Expert Opin Pharmacother,2004,5(5):1153-1162.
[9] Zheng D,Cui C,Yu M,et al. Coenzyme Q10 promotes osteoblast proliferation and differentiation and protects against ovariectomy-induced osteoporosis [J].Mol Med Rep,2018,17(1):400-407.
[10] Moon HJ,Ko WK,Jung MS,et al. Coenzyme q10 regulatesosteoclast and osteoblast differentiation [J]. JFood Sci,2013,78(5):H785-891.
[11] Wu X,Liang S,Zhu X,et al. Erratum:CoQ10 suppression of oxidative stress and cell senescence increases bone mass in orchiectomized mice [J]. Am J Transl Res,2021,13(4):3923.
[12] Li R,Jia Z,Trush MA. Defining ROS in Biology and Medicine [J]. React Oxyg Species(Apex),2016,1(1):9-21.
[13] Lee NK,Choi YG,Baik JY,et al. A crucial role for reactive oxygen species in RANKL-induced osteoclast differentiation [J]. Blood, 2005,106(3):852-859.
[14] Fraser JH,Helfrich MH,Wallace HM,et al. Hydrogen peroxide, but not superoxide,stimulates bone resorption in mouse calvariae [J]. Bone, 1996,19(3):223-226.
[15] Geng Q,Gao H,Yang R,et al. Pyrroloquinoline Quinone Prevents Estrogen Deficiency-Induced Osteoporosis by Inhibiting Oxidative Stress and Osteocyte Senescence [J]. IntJ Biol Sci,2019,15(1):58-68.
[16] Zhang XX,Qian KJ,Zhang Y,et al. Efficacy of coenzyme Q10 in mitigating spinal cord injury-induced osteoporosis [J]. Mol Med Rep,2015, 12(3):3909-3915.
[17] Amaya-Montoya M,Pérez-Londoño A,Guatibonza-García V, et al. Cellular Senescenceasa Therapeutic Target forAge-Related Diseases: A Review [J].Adv Ther,2020,37(4):1407-1424.
[18] Corrado A,Cici D,Rotondo C,et al. Molecular Basis of Bone Aging [J]. IntJ Mol Sci,2020,21(10):3679.
[19] Li X,Zhan J,Hou Y,et al. Coenzyme Q10 Regulation of Apoptosis and Oxidative Stress in H2O2 Induced BMSC Death by Modulating the Nrf-2/NQO-1 Signaling Pathway and Its Application in a Model of Spinal Cord Injury [J].Oxid Med Cell Longev,2019,2019:6493081.
[20] Zhang D,Yan B,Yu S,et al. Coenzyme Q10 inhibits the aging of mesenchymal stem cells induced by D-galactose through Akt/mTOR signaling [J].Oxid Med Cell Longev,2015,2015:867293.
[21] Wang Kexin, Chen Cailing, Zheng Xiaoyan, et al. Effects of coenzyme Q10 on bone microstructure and myofibrils in male mice caused by D-galactose [J]. Chinese Journal of Pharmacology, 2019, 35(11): 1544-1550.
[22] Varela-López A,Ochoa JJ,Llamas-Elvira JM,et al. Loss of Bone Mineral Density Associated with Age in Male Rats Fed on Sunflower Oil Is Avoided by Virgin Olive Oil Intake or Coenzyme Q Supplementation [J]. Int J Mol Sci,2017,18(7):1397.
[23] Kömürcü E,Oktay M,Kaymaz B,et al. Preventive effects of coenzyme Q10(CoQ10)on steroid-induced osteonecrosis in rats [J].Acta Orthop Traumatol Turc,2014,48(2):217-222.
[24] Hong Yan, Zheng Yangbin, Liu Bo. Experimental evaluation of the toxicological safety of coenzyme Q10 in mice [J]. Primary Care Forum, 2017, 21(25): 3461.
[25] Wu Keqin, Huang Jianping, Zhong Liyun, et al. Coenzyme Q10 toxicity study [J]. Strait Pharmacy, 2012, 24(8): 39-41.
[26] Honda K,Tominaga S,Oshikata T,et al. Thirteen-week repeated dose oral toxicity study of coenzyme Q10 in rats [J]. J Toxicol Sci,2007,32(4):437-448.
[27] McGarry A,McDermott M,Kieburtz K,et al. A randomized, double-blind,placebo-controlled trial of coenzyme Q10 in Huntington disease [J]. Neurology,2017,88(2):152-159.
[28] Apetauerova D,Scala SA,Hamill RW,et al. CoQ10 in progressive supranuclear palsy:A randomized,placebo-controlled,double-blind trial [J].Neurol Neuroimmunol Neuroinflamm,2016,3(5):e266.


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese








