Study on COQ10 Improves Left Ventricular Diastolic Insufficiency in Type 2 Diabetes
Diabetic cardiomyopathy is an independent cardiac complication in patients with diabetes mellitus (independent of myocardial ischemia and hypertension), characterized by diastolic and/or systolic dysfunction, which may be complicated by heart failure, arrhythmias, cardiogenic shock and sudden death[1] . Left ventricular diastolic dysfunction is a characteristic manifestation, and its pathogenesis involves a variety of pathophysiological mechanisms, including microvascular disease, myocardial fibrosis, interstitial inflammation, oxidative stress injury, and calcium homeostasis abnormality, etc.[1] .
However, a clear mechanism for this cardiac damage has not yet been fully elucidated. Many factors, including metabolic and oxidative free radicals, contribute to the formation of diabetic cardiomyopathy and provide new directions for the study of the etiology and treatment of diabetic cardiomyopathy.
Studies have shown that the levels of vitamin E quinone and lipid hyperoxidation in diabetic myocardial tissues are significantly higher than those in normal myocardial tissues, and high glucose levels can directly cause the production of oxidative free radicals and lead to lipid hyperoxidation of myocardial cell membranes[2] . Since myocardium has a lower content of free radical scavenging enzymes than other tissues, it is an easy target for free radicals and oxidative reactions, which strongly proves the role of free radicals in diabetic cardiomyopathy.
COQ10 is a fat-soluble quinone that acts as an important hydrogen transporter in the respiratory chain and is a key factor in the cellular energy production of living organisms, with antioxidant and intracellular oxygen flow control effects. Due to its free radical scavenging and antioxidant properties, Coenzyme Q10 has important applications in the treatment of cardiovascular diseases[3-4] .
Previous studies have concluded that coenzyme Q10 can delay the progression of heart failure in patients with cardiomyopathy, reduce the mortality rate, prolong life expectancy, and improve the quality of life of patients [4]; coenzyme Q10 can improve myocardial metabolism, and can be used for the treatment of angina pectoris caused by coronary artery stenosis [5]; coenzyme Q10 can also enhance the heart's ability to withstand hypoxia, and it is expected that coenzyme Q10 can be developed as a special-purpose healthcare agent [4]; coenzyme Q10 can lower vascular systolic pressure and diastolic pressure in the treatment of hypertensive disorders.

In the treatment of hypertension, coenzyme Q10 can reduce vascular systolic and diastolic blood pressure. Recently, coenzyme Q10 has been found to protect cardiomyocytes in diabetic animal models against high glucose-induced myocardial hypertrophy, oxidative stress and fibrosis[6] .
The aim of this study was to investigate whether coenzyme Q10 can improve the diabetic patients with combined left ventricular diastolic dysfunction and to examine the role of oxidative stress and inflammation.
1 Information and Methodology
1.1 General Information
Patients with type 2 diabetes mellitus who were hospitalized in the endocrinology department of the hospital were selected for the study and excluded from the study were hypertensive disease, coronary heart disease, heart valve disease, cardiomyopathy and other diseases. The diagnosis and typing of diabetes mellitus were in accordance with the latest ADA recommendations for the diagnosis of diabetes mellitus.
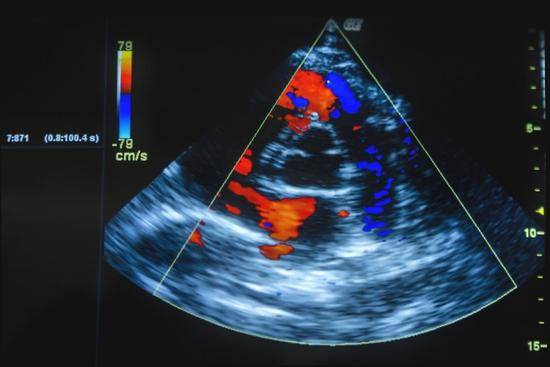
All patients underwent conventional 12-lead electrocardiogram or exercise electrocardiogram, color Doppler cardiac ultrasound, and some underwent coronary angiography or 64-slice CT coronary angiography. All patients were tested for glycated hemoglobin, blood lipids, and renal function; blood pressure and body mass index were recorded.
1.2 Ultrasound Evaluation Indicators
The parameters were measured by cardiac ultrasound (Sequoia-512 color Doppler ultrasound, 2MHz-3.5MHz, ACUSON) by the same experienced ultrasound specialist in a slight left lateral position, and the average of three measurements was taken. The main measurements included early diastolic peak flow rate (E) and late diastolic flow rate (A), and the left ventricular ejection fraction (LVEF) was calculated by the Simpson method. The diagnostic criteria for LV diastolic insufficiency were as follows: (1) typical signs and symptoms of heart failure; (2) normal LV ejection fraction (LVEF) (>45%), and normal left ventricular cavity size; (3) echocardiographic evidence of LV diastolic abnormality; and (4) absence of cardiac valvular disease and exclusion of pericardial disease, hypertrophic cardiomyopathy, or restrictive cardiomyopathy on echocardiographic examination. (iv) no valvular disease on echocardiography and exclusion of pericardial disease, hypertrophic cardiomyopathy or restrictive cardiomyopathy.
Grading of the severity of diastolic cardiac insufficiency: Class I: E/A ratio <0.75; Class II: E/A ratio 0.75. 1 . 50; Class III: E/A ratio > 1 .50.
1.3Grouping and Treatment
The patients were divided into the control group and the treatment group using a randomized table: the control group was given conventional diabetes treatment, including all kinds of hypoglycemic drugs, insulin injection, and so on. The treatment group was given coenzyme Q10 (Nembutalan, 10 mg, 3 times a day for 6 months) on the basis of the conventional treatment. Cardiac function tests, including ejection fraction and diastolic function, were performed before treatment, and these tests were repeated after treatment.
1.4 Blood Sample Collection
Venous blood samples were collected early in the morning of the next day after admission, and collected in test tubes anticoagulated with 1:9 sodium citrate. General tests such as blood routine, lipid profile, coagulation function, glycated hemoglobin, cardiac enzymes, brain natriuretic peptide, etc., were performed; plasma superoxide dismutase (SOD) and malondialdehyde (MDA) levels of oxygen radicals before and after the treatment were determined; total plasma SOD activity was measured by the o-phenylene bisabolol autoxidation rate; and plasma MDA levels were measured by the thiobarbituric acid method. The total plasma SOD activity was determined by the autoxidation rate of catechol, and the plasma MDA level was determined by the thiobarbituric acid method.
Comparison of the changes in the levels of high-sensitivity C-reactive protein (hs-CRP) and interleukin 6 (IL-6), which are indicators of inflammation, before and after treatment: hs-CRP was measured by latex immunoturbidimetric assay on a Shimadzu CL-7200 biochemical analyzer according to the instruction manual. Enzyme-linked immunosorbent assay (ELISA) was used for the determination of IL-6 levels, and the reagents were provided by Beijing Jingmei Biotechnology Company according to the instruction manual.

1.5 Statistical Methods
The data were analyzed by SPSS 16.0 statistical software. The data of continuous variables were expressed as x- ± s, and the t-test was used to compare the two groups; the data of categorical variables were expressed as rate or composition ratio, and the chi-square test was used to compare the data; the data of unequal variances were tested by rank-sum test. p<0.05 was regarded as the statistically significant difference.
2.Results
2.1 Baseline Data of the Two Groups of Patients
A total of 106 eligible patients, 60 men and 46 women, aged (67.2±9.5) years, with a body mass index of (24.5 3.7) kg/m2 were enrolled. There was no statistically significant difference (P>0.05) between the treatment group (53 patients) and the control group (53 patients) in terms of the main baseline clinical indicators and laboratory indicators, such as gender, smoking history, insulin therapy, low-density lipoprotein, glycated hemoglobin, and so on. Compared with the control group, patients in the treatment group had a longer duration of diabetes, and the diastolic function index was significantly reduced (P < 0.05). See Table 1.
Table 1 Baseline data of the two groups of patients (x- ±s)
Key indicators | Treatment group (n= 53) | Control group (n= 53) | P-value |
Advanced age (>75 years, %) | 13 .2 | 9 .4 | 0.066 |
Sex (male, %) | 58 .5 | 54.7 | 0.32 |
Body mass index (kg/m )2 | 24.8±4.7 | 24.3±4.1 | 0.22 |
Smoking history (%) | 26.4 | 22.6 | 0.55 |
Duration of diabetes (years) | 6.0±1 .2 | 2.2±1 .7 | 0.002 |
Insulin therapy (%) | 11 .3 | 7.54 | 0. 17 |
LDL-C (mmol/L) | 3 .9±3 .8 | 3 .3±3 .5 | 0. 11 |
HBA1C (%) | 0.97±0.25 | 0.81±0.21 | 0.057 |
LVEF (%) | 54±9 .6 | 55±11 . 1 | 0.25 |
E (cm/s) | 78±20 | 62±26 | 0.011 |
A (cm/s) | 75±19 | 83±21 | 0.022 |
SOD (kU/L) | 105±29 | 98±25 | 0.32 |
MDA (μmol/L) | 28±6 | 25±7 | 0.21 |
hs-CRP (mg/L) | 0.6±2. 1 | 0.5±3 .4 | 0.29 |
IL-6 (ng/L) | 4.9±2.8 | 4.3±2.5 | 0.44 |
Note: LDL-C: low-density lipoprotein cholesterol; HBA1C: glycosylated hemoglobin; LVEF: left ventricular ejection fraction; E: early diastolic peak flow rate; A: late diastolic flow rate; SOD: plasma superoxide dismutase; MDA: malondialdehyde; hs-CRP: high-sensitivity C-reactive protein; IL-6: interleukin-6.
2.2 Comparison of Left Ventricular Diastolic Function Between the Two Groups After 6 Months of Treatment
In the control group, early diastolic and late diastolic peak flow velocities were (59±28) cm/s and (81±23) cm/s, respectively, after 6 months of treatment, and the differences were not statistically significant compared with those before treatment (P>0.05); in the treatment group, early diastolic and late diastolic peak flow velocities were (69±21) cm/s and (66±22) cm/s, respectively, after 6 months of treatment, and the differences were statistically significant (P=0.012, P=0.021) compared with those before treatment. The differences were statistically significant (P=0.012, P=0.021).
2.3 Comparison of Oxidative Stress and Inflammation Indexes Between the Two Groups After 6 Months of Treatment
The changes in the levels of oxidative stress and inflammatory indexes in the two groups were shown in Table 2. In the treatment group, the serum oxidative stress indicators (SOD, MDA) and inflammation indicators (hs-CRP, IL-6) improved significantly (P<0.05) compared with the pre-treatment levels, while the control group showed little improvement (P>0.05).
Table 2 Changes in oxidative stress and inflammation indexes after 6 months of treatment in both groups of patients
Changes in indicators | Treatment group (n= 53) | Control group (n= 53) | P-value |
SOD (kU/L) MDA (μmol/L) hs-CRP (mg/L) IL-6 (ng/L) | - 25±19 - 0.21±1 . 12 1 .9±0.8 | 4±15 2±3 0.04±1 .41 0.3±0.5 | 0.012 0.021 0.039 0.014 |
Note:SOD: plasma superoxide dismutase; MDA: malondialdehyde; hs-CRP: high-sensitivity C-reactive protein; IL-6: interleukin-6.
3.Discussion
The results of this study showed that 6 months of treatment with coenzyme Q10 in type 2 diabetes mellitus patients with left ventricular diastolic insufficiency significantly improved early left ventricular diastolic dysfunction, accompanied by a significant reduction in serum oxidative stress and inflammatory markers. The accumulation of oxidative intermediates is an important pathogenic factor in diabetic cardiomyopathy. Evidence suggests that free radical-oxidizing defense enzymes such as catalase and superoxide dismutase (SOD) are compensatorily elevated in diabetic myocardial tissues as a result of oxidative stress[7] .
Researchers treated diabetic experimental animals with antioxidants such as Probuc01, superoxide dismutase and catalase, and found that the functional and morphological parameters of diabetic cardiomyopathy were greatly improved to varying degrees[7-8] . Many factors, including metabolic and oxidative free radicals, contribute to the development of diabetic cardiomyopathy. These studies have provided new directions not only for the etiology but also for the treatment of diabetic cardiomyopathy.

There is no direct evidence that coenzyme Q10 directly protects cardiomyocytes against diabetes-induced damage, but recent studies have found that coenzyme Q10 protects cardiomyocytes in diabetic animal models against hyperglycemia-induced myocardial hypertrophy, oxidative stress, and fibrosis[6] . Coenzyme Q10 is a free radical scavenger and antioxidant. From the perspective of improving oxidative stress and inflammation, using coenzyme Q10 as an entry point, it is expected to explore a new way to prevent diabetic cardiomyopathy.
In the present study, the left ventricular diastolic dysfunction of the patients improved significantly after treatment with coenzyme Q10, which is consistent with the findings of previous preclinical studies, and confirms the protective effect of coenzyme Q10 in diabetic myocardial injury, and its protective effect is related to the modulation of oxidative stress and inflammatory response.
In conclusion, coenzyme Q10 can improve left ventricular diastolic dysfunction in the early stage of type 2 diabetes mellitus, and its mechanism is related to the regulation of oxidative stress and inflammation, which may be a new pathway and a new target for the prevention and treatment of diabetic cardiomyopathy.
Reference:
[ 1] Bugger H , Abel ED . Molecular mechanisms of diabetic cardiomyopathy[J] . Diabetologia ,2014 ,57(4) :660-671 .
[2] Lorenzo O , Ramirez E , Picatoste B , et al. Alteration of energy substrates and ROS production in diabetic cardiomyopathy [ J ] . Mediators Inflamm , 2013 , 2013 : 461967.
[3] Parmar SS , Jaiwal A , Dhankher OP , et al. Coenzyme Q10 production in plants : current status and future prospects [J] . Crit Rev Biotechnol ,2013 :1-13 .
[4] Madmani ME , Solaiman AY , Tamr AK , et al. Coenzyme Q10 for heart failure[ J] . Cochrane Database Syst Rev , 2014 ,9(6) :D8684.
[5] Zeb I , Ahmadi N , Nasir K , et al. Aged garlic extract and coenzyme Q10 have favorable effect on inflammatory markers and coronary atherosclerosis progression : A randomized clinical trial[J] . J Cardiovasc Dis Res , 2012 , 3(3) :185-190.
[6] Dzugkoev SG , Kaloeva MB , Dzugkoeva FS . Effect of combination therapy with coenzyme Q10 on functional and metabolic parameters in patients with type 1 diabetes mellitus[J] . Bull Exp Biol Med ,2012 ,152(3) :364-366.
[7] Acharya JD , Pande AJ , Joshi SM , et al. Treatment of hyperglycemia in newly diagnosed diabetic patients is associated with a reduction in oxidative stress and
improvement in beta-cell function[J] . Diabetes Metab Res Rev , 2014. doi : 10. 1002/dmrr.2526.
[8] Kim MJ , Chung JY , Kim JH , et al. Effects of cranberry powder on biomarkers of oxidative stress and glucose control in db/db mice[J] . Nutr Res Pract , 2013 , 7(6) : 430-438 .


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese






