What Is the Use of Turmeric Curcumin in Periodontitis?
Periodontitis is a chronic inflammation caused by local factors such as dental plaque. Mechanical treatments such as supragingival scaling and subgingival curettage are often used, but the morphology of the tooth surface or limitations of the instruments sometimes prevent complete removal of the infectious material. Therefore, drug therapy has become one of the most commonly used adjunctive methods for mechanical treatment. Adjuvant drugs can inhibit the activity of pathogenic bacteria, regulate the host inflammatory response, etc., thereby enhancing the effect of mechanical treatment and restoring periodontal health. Common adjuvant drugs include antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs) [1]. However, antibiotics can easily lead to the development of drug-resistant strains or dysbiosis, while NSAIDs may increase the risk of persistent bleeding or the occurrence of hematomas. Therefore, there is an urgent need to discover new adjuvant drugs that are both effective and safe.
Natural plant extracts have the advantages of being cost-effective and having few side effects, and have gradually become a research hotspot [2]. Curcumin is an active polyphenol extracted from the plants turmeric and galangal, and has anti-inflammatory, antioxidant, antibacterial and wound-healing effects [3]. Periodontal destruction is caused by direct damage from plaque microorganisms and indirect damage from the excessive immune response they trigger. Therefore, curcumin's antibacterial and anti-inflammatory effects can be used to treat periodontitis. However, low bioavailability limits the complete translation of curcumin's in vitro benefits into clinical applications. Therefore, different drug delivery systems such as liposomes, nanoparticles, solid dispersions, emulsions, micelles, etc. have been developed and applied [4]. This article reviews the mechanism of curcumin in the prevention and treatment of periodontitis and the different delivery strategies of curcumin, with the aim of providing ideas for basic research and clinical applications of curcumin in the prevention and treatment of periodontitis.

I. The pharmacological effects of curcumin on periodontitis
1. Antibacterial effect
Curcumin has a strong antibacterial effect and can exert a bacteriostatic effect through a variety of antibacterial mechanisms, such as affecting the permeability of cell membranes, the expression of bacterial division proteins and virulence factor genes, etc. Bocher et al. [5] constructed an in vitro biofilm model by implanting an artificial periodontal pocket around a titanium rod and introducing various pathogenic bacteria extracted from the patient's gingival sulcus. They found that the total bacterial count treated with curcumin was reduced by 97.35% (P < 0.05), which was significantly stronger than the control group.
Further studies showed that curcumin can inhibit the growth of periodontal pathogens such as Porphyromonas gingivalis (P. gingivalis), Fusobacterium nucleatum and Tannerella forsythia. Among them, 20 mg/mL curcumin can inhibit the growth of P. gingivalis biofilm by 80%, and the dose-dependent inhibition of P. gingivalis virulence factors (gingipain R and gingipain K) activity [6]. Moreover, curcumin and its derivatives can be inserted into the phospholipid bilayer to increase membrane permeability, and can also inhibit bacterial division by inhibiting the important protein FtsZ, which supplies energy and drives division during bacterial division. This gives curcumin membrane permeability activity and broad-spectrum antibacterial activity, which can be used in combination with antibiotics to improve antibiotic uptake and increase efficacy [7].
2. Anti-inflammatory effect
Curcumin has active anti-inflammatory activity and can be a natural drug option for host inflammation regulation. Curcumin has been shown at the molecular level to inhibit inflammatory factors such as pro-inflammatory cytokines (interleukin, IL) by regulating signal pathways such as NF-κB [8], Janus kinase (Janus kinase, JAK)/signal transducer and activator of transcription (signal transducer and activator of transcription, STAT), mitogen-activated protein kinases (MAPK) [9], etc., inhibits the inflammatory factors such as pro-inflammatory cytokines (interleukins, ILs) -1β and IL-6 and tumor necrosis factor (tumor necrosis factor, TNF) -α, etc., and exerts an anti-inflammatory effect, inhibiting the progression of periodontitis [10]. The NF-κB pathway is one of the main pathways. When stimulated, NF-κB binds to the promoter region of the target gene through a cascade reaction, promoting the transcriptional expression of inflammatory factors.
Modulating NF-κB signal transduction and IL secretion is the most important functional mechanism of curcumin in regulating inflammatory bodies [8]. Curcumin can upregulate the suppressor of cytokine signaling (SOCS)-1 to reduce the expression of the JAK2/STAT3 signaling pathway, thereby downregulating the expression of inflammatory factors to inhibit inflammation [11]. For example, in colitis, curcumin can alleviate colitis symptoms and inhibit dendritic cells by inducing SOCS1 and SOCS3 to downregulate JAK2, STAT3 and STAT6 [12]. Inhibiting the STAT signaling pathway can reduce the expression and level of inflammatory cytokines, thereby reducing diseases caused by inflammatory responses. In addition, curcumin effectively inhibits the expression of inflammatory cytokines in LPS-induced macrophages by regulating the expression and activity of SOCS-1 and SOCS-3 and p38 MAPK [9]. Moreover, curcumin can significantly reduce inflammatory pain by inhibiting the JNK/MAP signal pathway in nerve cells [13].
Xiao et al. [14] demonstrated in a rat model of periodontitis induced by ligation that curcumin can inhibit NF-κB activation and reduce the production of IL-1β, PGE2, and TNF-α, thereby significantly reducing inflammatory cell infiltration. In addition, Diomede et al. [15] found that in vitro experiments showed that curcumin may act on periodontal stem cells through a novel mechanism of reactive oxygen species (ROS) cascade, namely Toll-like receptor 4/myeloid differentiation factor 88/NF-κB/inflammasome NLRP3/cysteine aspartate protease 1/IL-1β signaling pathway, thus becoming a new target drug for restoring homeostasis within tissues.
3.Osteoprotective effect
Curcumin has a strong osteoprotective effect, mainly by inhibiting inflammatory bone loss and promoting stem cell proliferation and differentiation. Curcumin reduces the inflammatory response and resorption of the alveolar bone by inhibiting TNF-α, IL-6, and other NF-κB receptor activators (receptor activator of nuclear factor-κB, RANK) and RANK ligand (receptor activator of nuclear factor-κB ligand, RANKL), reducing the inflammatory response and resorption of the alveolar bone [16]. RANKL induces osteoclast differentiation and is the main regulator of bone metabolism and the key to the mechanism of alveolar bone destruction in periodontitis.
In vitro experiments in gingival fibroblasts found that curcumin corrected the decrease in the osteoprotegerin/RANKL ratio induced by LPS, and further testing of periodontitis rats fed curcumin found that alveolar bone loss was reduced and collagen fiber decomposition was weakened [14]. Bakir et al. [10] hypothesized that curcumin inhibits T cell differentiation, thereby reducing osteoclastogenesis. In addition, human periodontal ligament stem cells can differentiate into osteoblasts to promote alveolar bone regeneration. Excessive production of ROS in chronic inflammation disrupts redox homeostasis, leading to cell damage and apoptosis and inhibiting bone differentiation. Studies have found that curcumin pretreatment can protect stem cells from oxidative stress, promote cell proliferation and osteogenic differentiation [17].
II. In vivo pharmacokinetics and safety of curcumin
1. Absorption and distribution of curcumin
The oral absorption rate of curcumin is extremely low and its distribution is limited. The maximum plasma concentration of curcumin in rats after oral administration of 2 g/kg is 1.35 μg/mL, the maximum plasma concentration of curcumin in mice after oral administration of 1 g/kg is 0.22 μg/mL, and the maximum plasma concentration of curcumin in volunteers after oral administration of 12 g is 0.051 μg/mL [18]. This may be due to the fact that curcumin is not water-soluble, is poorly absorbed in the digestive tract, is also subject to first-pass elimination by the liver, and most of the curcumin that enters the lower digestive tract is rapidly metabolized or excreted, resulting in extremely low blood concentrations. Coupled with the fact that curcumin is easily bound to plasma proteins, its distribution in tissues is limited. In mice injected intraperitoneally with 0.1 g/kg curcumin, the content of curcumin in the intestine reached a maximum value (0.117 g/kg), and the content of curcumin in the spleen, liver, kidney and brain was 0.0261 g/kg, 0.0269 g/kg, 0.0075 g/kg and 0.0004 g/kg, respectively [19].
2. Metabolism and excretion of curcumin
Curcumin is metabolized quickly in the body, mainly in the liver and intestines, and excreted in the feces. In mice orally administered with 1 g/kg curcumin, the plasma curcumin concentration decreased rapidly after 1 h and dropped below the detection limit (5 × 10-9 g/mL) within 6 h [19]. Burapan et al. [20] further found in vitro that curcumin was demethylated by the human intestinal bacterium Blautia sp. MRG-PMF1 to demethylcurcumin, and then demethylated to demethylcurcumin. After oral administration, most curcumin is excreted in the feces, and a small amount is absorbed in the intestine and rapidly metabolized in the liver and plasma [18]. After oral administration of 1 g/kg curcumin to rats, about 75% was excreted in the feces, while the amount in the urine was negligible [21].
3.Safety of curcumin
As a substance classified by the FDA as generally recognized as safe [22], curcumin is highly safe. No significant toxic effects were found in rats when they were given curcumin orally up to 5 g/kg, and no teratogenic or carcinogenic effects were found in long-term studies lasting more than three generations, nor was there any damage to reproductive capacity [19]. The first phase of clinical trials showed that curcumin is safe in humans even at high doses (12 g/d), and no significant adverse reactions were found in volunteers [23]; curcumin preparations at a dose of 0.5 g, taken orally twice a day for 30 days, are safe for humans [24].

III. Common delivery systems for curcumin
Different strategies such as increasing curcumin solubility, synthesizing curcumin nanodrugs, combining adjuvants, synthesizing new curcumin derivatives and analogues, and designing curcumin hybrid molecules have all been used to improve the bioavailability of curcumin [25]. Among these strategies, liposomes, nanoparticles, adjuvants, micelles, and hydrogels are the most widely used. Table 1 shows the commonly used delivery systems for curcumin and a comparison of the characteristics of different delivery systems.
1. Liposomes
Liposomes are artificially constructed spherical bilayer vesicles [26]. Encapsulation in liposomes can significantly improve the physicochemical properties of curcumin. Curcumin liposomes coated with bovine serum albumin were constructed as a long-circulating drug delivery system, which has the characteristics of low phagocytosis, sustained release, enhanced stability, and non-toxicity [27]. In addition, the development of targeted liposomal formulations can further improve the efficacy of curcumin. Barattin [28] and others prepared a new type of pH-sensitive liposome, modified with tetraarginine-distearoylglycerol and its pegylated counterpart, which contains a pH-sensitive polyanionic block. In the acidic environment of tumors, the arginine moiety is easily exposed, enhancing the targeted binding of liposomes to cancer cells.
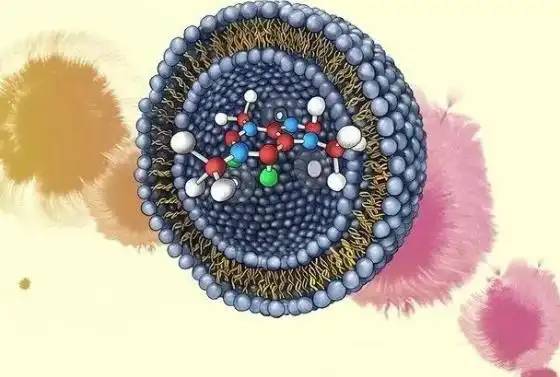
2. Nanoparticles
Nanoparticle drug delivery systems can improve the solubility of hydrophobic drugs. At the same time, the small particles can prolong the retention time of the drug in the body circulation and change the distribution, and allow targeted and trans-barrier transport [29]. Curcumin was encapsulated in solid lipid nanoparticles using an emulsification cryogelation method to increase intracellular curcumin concentrations and its accumulation in mitochondria, as well as improve its aqueous solution stability, in order to enhance the therapeutic activity of curcumin [30]. Twelve volunteers orally administered a γ-cyclodextrin curcumin preparation and curcumin, respectively. Compared with direct oral administration of curcumin, the γ-cyclodextrin curcumin preparation resulted in higher plasma curcumin concentrations, enhanced curcumin absorption, and significantly improved bioavailability [31]. Currently, common nanoparticles also include mesoporous silica nanoparticles and protein-based nanocarriers [32], which can also be used in the future to improve the bioavailability of curcumin.
3. Adjuvants
Adjuvants can alter the metabolism of curcumin and thus indirectly improve its bioavailability, such as piperine, lecithin and sesamin. In vivo metabolism involves the transfer of glucuronic acid groups to the hydroxyl groups of curcumin to form glucuronides, which are less active and are excreted more easily. Piperine is an inhibitor of glucuronic acid acidification in the liver and intestines [33]. It mainly improves the bioavailability of curcumin by inhibiting the aldehyde oxidation of curcumin by glucuronosyltransferase. Curcumin and piperine were given to rats with an artificially constructed periodontitis model. It was found that compared with the curcumin group alone, the combined application significantly reduced the activity of NF-κB in periodontal tissues, reduced the infiltration of inflammatory cells, increased collagen content, and had the potential to promote periodontitis soft tissue healing and bone tissue mineralization [34]. Further in vitro experiments found that curcumin in combination with piperine can inhibit the expression of osteoclast-specific markers tartrate-resistant acid phosphatase (TRAP), cathepsin K and calcitonin receptor, reduce osteoclastogenesis, and have no toxic effect on periodontal ligament cells [35].
4. Micelles
Micelles refer to ordered aggregates of molecules formed by surfactants in aqueous solutions, consisting of a hydrophilic shell and a hydrophobic core, which can load hydrophobic drugs. Nanometer-scale micelles can spill over from the blood vessel wall into cells, and the hydrophilic shell of the micelle can escape removal by the reticuloendothelial system, prolonging the circulation time of the drug. Curcumin polylactic-polyglycolic acid nanomicelles were prepared, and their antibacterial activity against Pseudomonas aeruginosa was investigated. It was found that compared with free curcumin, curcumin micelles can better penetrate biofilms and effectively destroy them, enhancing the antibacterial effect of curcumin [36]. Lee D et al. [37] designed an acid-responsive curcumin polymer conjugated by 1,4,4'-trimethylenedipiperidine and polyethylene glycol acrylate. After incorporating curcumin into its hydrophobic backbone, it self-assembles into micelles under aqueous conditions due to its amphiphilicity, and rapidly releases curcumin under acidic conditions. The problem of poor water solubility of curcumin is solved, and it has the ability to stimulate pathological reactions, achieving controlled release.
5. Hydrogel
A hydrogel is a semi-solid gel with water as the dispersing medium. It usually has a hydrophilic three-dimensional network structure, which can achieve the advantages of slow-release curcumin, strong mucosal affinity, and long local retention time. It is suitable for use as a transdermal or mucosal drug delivery system. Hydroxypropyl-β-cyclodextrin was used to improve the solubility of curcumin, which was loaded into a bacterial cellulose hydrogel. It significantly inhibited staphylococcus, and also had blood compatibility, cell compatibility and antioxidant properties [38]. Poloxamer F 127 was used as a temperature-sensitive polymer, and Popul P 934 was used as a pH-sensitive polymer to a controlled-release curcumin hydrogel was formulated. In vitro experiments showed that the gel was easy to insert into periodontal pockets and controlled the release of drugs for a long time. Further clinical trials found that after scaling and root planing in patients with periodontitis, the application of the gel significantly reduced the periodontal probing depth and bleeding index compared with no gel, and improved patient compliance [39].
IV. Clinical application of curcumin
In clinical studies, the use of curcumin as an adjunct to periodontal treatment can significantly reduce periodontal inflammation. Ravishankar et al. [45] selected periodontitis patients and applied curcumin gel and ornidazole gel respectively. At the one-month evaluation, curcumin gel had a better therapeutic effect than ornidazole gel, and the depth of periodontal pockets, plaque index and clinical attachment loss were significantly reduced. Pulikkotil et al. [46] selected healthy subjects and applied curcumin, chlorhexidine and chlorhexidine-metronidazole gel as the only method of maintaining oral hygiene to construct a 29-day gingivitis model, periodontal status and changes in IL-1β and mucosal-associated epithelial chemokine (MEC/C-C motif chemokine 28, CCL28) in gingival crevicular fluid were evaluated. It was found that the periodontal status in the curcumin group was comparable to that in the chlorhexidine-metronidazole gel group, but IL-1β and CCL28 were significantly lower than those in the chlorhexidine gel group.

In addition, a meta-analysis of nine randomized controlled trials involving 420 participants/sites [47] showed that curcumin had a similar effect on reducing the depth of periodontal pockets, clinical attachment loss, gingival index and plaque index as chlorhexidine, which was also used as an adjuvant drug. Another meta-analysis evaluating the effect of curcumin mouthwash on plaque and gingival index also reached similar conclusions, with curcumin and chlorhexidine having comparable efficacy in reducing plaque (CI: -0.53, 1.07, P=0.51) and gingival index (CI: -0.35, 0.09, P=0.24) [48]. Chlorhexidine is currently the “gold standard” drug for adjuvant periodontal medication. Curcumin is comparable to it in efficacy, which indicates that curcumin plays an important role in inhibiting periodontal pathogenic bacteria, reducing the degree of inflammation, and improving periodontal clinical indicators.
References
[1] Guan Lifan, Wang Mi. Research progress in the drug treatment of chronic periodontitis [J]. Medical Review, 2021, 27(2): 334-338.
[2] Soleimani V, Sahebkar A, Hosseinzadeh H. Turmeric (Curcuma longa) and its major constituent (curcumin) as nontoxic and safe substances: Review [J]. Phytotherapy research: PTR, 2018, 32(6): 985-995.
[3]Mirzaei H, Shakeri A, Rashidi B, et al. Phytosomal curcumin: A review of pharmacokinetic, experimental and clinical studies [J]. Biomedicine & Ppharmacotherap, 2017, 85: 102-112.
[4]Ma Z, Wang N, He H, et al. Pharmaceutical strategies of improving oral systemic bioavailability of curcumin for clinical application[J]. Journal of controlled release: official journal of the Controlled Release Society, 2019, 316: 359-380.
[5]Bocher S, Wenzler JS, Falk W, et al. Comparison of different laser-based photochemical systems for periodontal treatment[J]. Photodiagnosis and Photodynamic Therapy, 2019, 27: 433-439.
[6]zui S, Sekine S, Maeda K, et al. Antibacterial activity of curcumin against periodontopathic bacteria[J]. J Periodont, 2016, 87(1): 83-90.
[7]Polaquini CR, Morão LG, Nazaré AC, et al. Antibacterial activity of 3, 3 '-dihydroxycurcumin (DHC) is associated with membrane perturbation[J]. Bioorganic chemistry, 2019, 90: 103031.
[8]Hasanzadeh S, Read MI, Bland AR, et al. Curcumin: an inflammasome silencer[J]. Pharmacological Research, 2020, 159: 104921.
[9]Guimarães MR, Leite FRM, Spolidorio LC, et al. Curcumin abrogates LPS-induced pro-inflammatory cytokines in RAW 264.7 macrophages. Evidence for novel mechanisms involving SOCS-1, -3 and p38 MAPK[J]. Archives of Oral Biology, 2013, 58(10): 1309-1317.
[10]Bakir B, Ay ZY, Buyukbayram HI, et al. Effect of curcumin on systemic T helper 17 cell response; gingival expressions of interleukin-17 and retinoic acid receptor-related orphan receptor gamma t; and alveolar bone loss in experimental periodontitis[J]. J Periodont, 2016, 87(11): E183-E191.
[11]Ashrafizadeh M, Rafiei H, Mohammadinejad R, et al. Potential therapeutic effects of curcumin mediated by JAK/STAT signaling pathway: A review[J]. Phytotherapy research: PTR, 2020, 34(8): 1745-1760.
[12]Zhang X, Wu J, Ye B, et al. Protective effect of curcumin on TNBS-induced intestinal inflammation is mediated through the JAK/STAT pathway[J]. BMC Complementary and Alternative Medicine, 2016, 16(1): 299.
[13]Uddin SJ, Hasan MF, Afroz M, et al. Curcumin and its multi- target function against pain and inflammation: an update of pre-clinical data[J]. Curr Drug Targets, 2021, 22(6): 656-671.
[14]Xiao CJ, Yu XJ, Xie JL, et al. Protective effect and related mechanisms of curcumin in rat experimental periodontitis [J]. Head & Face Medicine, 2018, 14(1): 12.
[15]Diomede F, Fonticoli L, Guarnieri S, et al. The Effect of liposomal curcumin as an anti-inflammatory strategy on lipopolysaccharide e from porphyromonas gingivalis treated endothelial committed neural crest derived stem cells: morphological and molecular mechanisms[J]. International Journal of Molecular Sciences, 2021, 22(14): 7534.
[16]Mau LP, Cheng WC, Chen JK, et al. Curcumin ameliorates alveolar bone destruction of experimental periodontitis by modulating osteoclast differentiation, activation and function[J]. Journal of Functional Foods, 2016, 22: 243-256.
[17]Tan L, Cao Z, Chen H, et al. Curcumin reduces apoptosis and promotes osteogenesis of human periodontal ligament stem cells under oxidative stress in vitro and in vivo[J]. Life Sciences, 2021, 270: 119125.
[18]Hassanzadeh K, Buccarello L, Dragotto J, et al. Obstacles against the Marketing of Curcumin as a Drug[J]. International Journal of Molecular Sciences, 2020, 21(18): 6619.
[19]Anand P, Kunnumakkara AB, Newman RA, et al. Bioavailability of curcumin: Problems and promises[J]. Molecular Pharmaceutics, 2007, 4(6): 807-818.
[20]Burapan S, Kim M, Han J. Curcuminoid demethylation as an alternative metabolism by human intestinal microbiota [J].
Journal of Agricultural and Food Chemistry, 2017, 65(16): 3306-3311.
[21]Scazzocchio B, Minghetti L, D'archivio M. Interaction between gut microbiota and curcumin: a new key of understanding for the health effects of curcumin[J]. Nutrients, 2020, 12(9): 2499.
[22]Kocaadam B, Sanlier N. Curcumin, an active component of turmeric (Curcuma longa), and its effects on health [J]. Critical Reviews in Food Science and Nutrition, 2017, 57(13): 2889-2895.
[23]Patel SS, Acharya A, Ray RS, et al. Cellular and molecular mechanisms of curcumin in prevention and treatment of disease[J]. Crit Rev Food Sci Nutr, 2020, 60(6): 887-939.
[24]Soleimani V, Sahebkar A, Hosseinzadeh H. Turmeric (Curcuma longa) and its major constituent (curcumin) as nontoxic and safe substances: Review [J]. Phytotherapy Research, 2018, 32
(6): 985-995.
[25]Noureddin SA, El-Shishtawy RM, Al-Footy KO. Curcumin analogues and their hybrid molecules as multifunctional drugs [J]. European Journal of Medicinal Chemistry, 2019, 182: 111631.
[26] Wan L, Jin H, Wu X, et al. In vitro study of the effect of liposome-mediated NELL1 gene on adipose stem cells. Modern Stomatology Journal, 2015, 29(3): 161-165.
[27]Wei XQ, Ba K. Construction a long-circulating delivery system of liposomal curcumin by coating albumin[J]. ACS omega, 2020, 5(27): 16502-16509.
[28]Barattin M, Mattarei A, Balasso A, et al. pH-Controlled liposomes for enhanced cell penetration in tumor environment [J]. ACS Appl Mater Interfaces, 2018, 10(21): 17646-17661.
[29] Wang N, Song XQ, Liu H, et al. Research progress of polydopamine-modified biomedical materials [J]. Modern Stomatology, 2017, 31(2): 113-116.
[30]Jiang S, Zhu R, He X, et al. Enhanced photocytotoxicity of curcumin delivered by solid lipid nanoparticles [J]. International Journal of Nanomedicine, 2017, 12: 167-178.
[31]Purpura M, Lowery RP, Wilson JM, et al. Analysis of different innovative formulations of curcumin for improved relative oral bioavailability in human subjects[J]. European Journal of Nutrition, 2018, 57(3): 929-938.
[32]Chen Y, Lu Y, Lee RJ, et al. Nano encapsulated curcumin: and its potential for biomedical applications[J]. International Journal of Nanomedicine, 2020, 15: 3099-3120.
[33]Lewandowska U, Szewczyk K, Hrabec E, et al. Overview of metabolism and bioavailability enhancement of polyphenols [J]. J Agric Food Chem, 2013, 61(50): 12183-12199.
[34]Guimaraes-Stabili MR, De Aquino SG, De Almeida Curylofo F, et al. Systemic administration of curcumin or piperine enhances the periodontal repair: a preliminary study in rats[J]. Clin Oral Investig, 2019, 23(8): 3297-3306.
[35]Martins CA, Leyhausen G, Volk J, et al. Curcumin in combination with piperine suppresses osteoclastogenesis in vitro [J]. Journal of Endodontics, 2015, 41(10): 1638-1645.
[36]Barros CHN, Hiebner DW, Fulaz S, et al. Synthesis and self-assembly of curcumin-modified amphiphilic polymeric micelles with antibacterial activity [J]. Journal of Nanobiotechnology, 2021, 19(1): 104.
[37]Kang C, Jung E, Hyeon H, et al. Acid-activatable polymeric curcumin nanoparticles as therapeutic agents for osteoarthritis [J]. Nanomedicine: Nanotechnology, Biology, and Medicine, 2020, 23: 102104.
[38]Gupta A, Keddie DJ, Kannappan V, et al. Production and characterisation of bacterial cellulose hydrogels loaded with curcumin encapsulated in cyclodextrins as wound dressings [J]. European Polymer Journal, 2019, 118: 437-450.
[39]Nasra MM, Khiri HM, Hazzah HA, et al. Formulation, in-vitro characterization and clinical evaluation of curcumin in-situ gel for treatment of periodontitis[J]. Drug delivery, 2017, 24
(1): 133-142.
[40] Zhang Xinjian, Zhang Bin. Research progress in the application of nanoparticle drug delivery systems in the local drug treatment of periodontitis [J]. Oral Disease Prevention and Control, 2022, 30(1): 73-76.
[41]He C, Zhang X, Yan R, et al. Enhancement of cisplatin efficacy by lipid-CaO(2) nanocarrier-mediated comprehensive modulation of the tumor microenvironment[J]. Biomater Sci, 2019, 7(10): 4260-4272.
[42]Srivastava S, Mohammad S, Pant AB, et al. Co-delivery of 5- Fluorouracil and curcumin nanohybrid formulations for improved chemotherapy against oral squamous cell carcinoma [J]. Journal of Maxillofacial and Oral Surgery, 2018, 17(4): 597-610.
[43]Trigo-Gutierrez JK, Vega-Chacón Y, Soares AB, et al. Antimicrobial activity of curcumin in nanoformulations: a comprehensive review[J]. International Journal of Molecular Sciences, 2021, 22(13): 7130.
[44]Das S, Parandhaman T, Dey MD. Biomolecule assisted synthesis of biomimetic nanocomposite hydrogel for hemostatic and wound healing application[J]. Green Chemistry, 2021, 23
(7): 629-669.
[45]Ravishankar PL, Kumar YP, Anila EN, et al. Effect of local application of curcumin and ornidazole gel in chronic periodontitis patients[J]. International Journal of Pharmaceutical Investigation, 2017, 7(4): 188-192.
[46]Pulikkotil S NS. Effects of curcumin on crevicular levels of IL ‐ 1β and CCL28 in experimental gingivitis[J]. Australian Dental Journal, 2015, 60(3): 317-327.
[47]Zhang Y, Huang L, Mazurel D, et al. Clinical efficacy of curcumin versus chlorhexidine as an adjunct to scaling and root planing for the treatment of periodontitis: A systematic review and meta-analysis[J]. Phytotherapy Research: PTR, 2021, 35(11): 5980-5991.
[48]Al-Maweri SA, Alhajj MN, Deshisha EA, et al. Curcumin mouthwashes versus chlorhexidine in controlling plaque and gingivitis: A systematic review and meta-analysis[J]. Int J Dent Hyg, 2022, 20(1): 53-61.


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese