What Is the Benefit of Rosmarinic Acid?
Rosmarinic acid is a phenolic acid compound of natural origin, formed by the condensation of caffeic acid and 3,4-dihydroxyphenyl lactic acid [1]. Its structural formula is shown in Figure 1. Rosmarinic acid is widely distributed, especially in the Boraginaceae, Lamiaceae, and Cucurbitaceae families [2-3]. It was first isolated and purified from Rosmarinus officinalis Linn by Italian chemists and named rosmarinic acid [4]. As an important polyphenolic antioxidant, rosmarinic acid has a wide range of applications in food and cosmetics [5-6], and it also has good pharmacological activities such as anti-inflammatory, antibacterial, and anticancer [7], so it has attracted widespread attention.
However, the deficiencies in the physical and chemical properties of rosmarinic acid have resulted in its low bioavailability. The main dosage forms currently used in research are powder and aqueous solution, which cannot meet the needs of clinical medication. Drug delivery technology can improve the shortcomings of the physical and chemical properties of therapeutic drugs, enhance delivery to diseased sites, improve treatment effects, and thus promote drug development and patient compliance. Therefore, this paper reviews the pharmacological effects of rosmarinic acid and the research progress of new drug delivery, providing a reference for the development and clinical application of rosmarinic acid.

1 Pharmacological effects of rosmarinic acid
1.1 Antioxidant effects
Reactive oxygen species include superoxide anions, peroxides, hydroxyl radicals and singlet oxygen. These molecules can affect cell survival signals and damage DNA [7]. Oxidative stress is an imbalance between intracellular oxidants and antioxidants, which leads to cell damage. Previous studies have shown that diseases such as Alzheimer's disease [8] and chronic obstructive pulmonary disease [9] are closely related to oxidative stress. In recent years, the potential of natural molecules to inhibit the production of free radicals or remove free radicals has attracted widespread attention. As an important natural phenolic acid compound, rosmarinic acid has good antioxidant properties due to the presence of a hydroxyphenolic group and a conjugated double bond at the C-3 position in its structure. Its oxidation capacity is higher than that of chlorogenic acid, vitamin E and caffeic acid [10-11].
Rosmarinic acid can exert its antioxidant activity through various pathways, scavenging nitrogen and oxygen free radicals, reducing the production of reactive oxygen species, degrading pro-oxidant compounds, and increasing antioxidant molecules such as glutathione; it also activates nuclear factor E2-related factor 2, which in turn activates the corresponding antioxidant enzymes [12]. Vostálová et al. [13] showed that rosmarinic acid can significantly reduce the production of reactive oxygen species and and reduced the secretion of interleukin-6 (IL-6) by T cells and macrophages, thereby preventing the production of human keratinocytes caused by UVB radiation.
1.2 Anti-inflammatory effect
Inflammation is the body's defence response to stimuli and is usually manifested as redness, swelling, heat, pain and dysfunction. Numerous studies have demonstrated that rosmarinic acid has a good anti-inflammatory effect. Complement activation often occurs at the site of inflammation, and rosmarinic acid can covalently bind to the active complement substance C3b to inhibit complement activity without side effects [14]. Cyclooxygenase-2 (COX-2) is a dangerous inflammatory factor. Scheckel et al. [15] found that rosmarinic acid can inhibit the expression of the COX-2 gene in colon cancer cells and benign mammary epithelial cells. Lembo et al. [16] demonstrated that rosemary acid can prevent damage induced by medium-wave ultraviolet radiation in a human keratinocyte cell line, reduce the production of inflammatory mediators such as tumor necrosis factor-α (TNF-α), IL-6, IL-8, and monocyte chemotactic protein 1, and promote the production of the protective IL-10.
In addition, Rocha et al. [17] established a model of local inflammatory edema in the feet of rats induced by carrageenan, a model of hepatic ischemia/reperfusion, and a model of systemic inflammatory thermal injury. The anti-inflammatory activity of rosmarinic acid was evaluated after oral or intravenous administration. Compared with the control group, the edema in the feet of rats in the rosmarinic acid treatment group was reduced by about 60%. possibly due to its anti-inflammatory activity by reducing the expression of pro-inflammatory factors TNF-α, IL-6 and IL-1β. In the hepatic ischemia-reperfusion model, rosmarinic acid can significantly reduce the plasma concentrations of alanine aminotransferase, glutamate transferase and lactate dehydrogenase. In a systemic inflammatory heat injury model, rosmarinic acid can reduce the markers of multiple organ dysfunction by regulating matrix metalloproteinases 9 (MMP9) and nuclear factor-κB (NF-κB). Ghasemzadeh Rahbardar et al. [18] studied the effect of rosmarinic acid on the neuroinflammatory environment in a mouse model of neuropathic pain and found that rosmarinic acid can regulate neuroinflammation by reducing inflammatory factors and oxidative markers such as COX-2, IL-1β, prostaglandin E2 and MMP2.
1.3 Antitumor effect
Cancer is known to be a serious threat to human health. Rosemary extract has a regulatory effect on various cancers, including colon cancer, liver cancer, and breast cancer. Cao et al. [19] found that rosemary extract can inhibit inflammatory cytokines and the NF-κB pathway in the tumor microenvironment, thereby exerting a therapeutic effect on liver cancer. It can also regulate the CD4+/CD8+ value and the secretion of IL-2 and γ-interferon, inhibit IL-6 and IL-10 expression, downregulate B-cell lymphoma 2 (Bcl-2), and upregulate Bcl-2 associated X protein (Bax) and caspase-3 expression, thereby effectively inhibiting tumor growth. Li Hong et al. [20] found in an in vitro cell experiment that rosmarinic acid can downregulate the Bcl-2 gene and upregulate the Bax gene, thereby inhibiting the proliferation and migration of human breast cancer cells and inducing apoptosis of tumor cells.
Karthikkumar et al. [21] used a 1,2-dimethylhydrazine-induced rat colon cancer model and found that rosmarinic acid can regulate pre-colon cancer lesions by affecting the levels of antioxidant enzymes in rats. Saiko et al. [22] used rosmarinic acid to treat human leukemia HL-60 cells and found that rosmarinic acid can effectively inhibit tumor cell proliferation and promote apoptosis by inhibiting the activity of nucleotide reductase and reduce dNTP production, thereby effectively inhibiting tumor cell proliferation and promoting apoptosis. Han et al. [23] found that rosmarinic acid inhibits tumor cell invasion and migration by inducing the phosphorylation of adenosine monophosphate activated protein kinase (AMPK), reduces the expression of MMP2 and MMP9, decreasing adhesion and the expression of adhesion molecules such as intercellular adhesion molecule-1 and integrin β1, thereby inhibiting colorectal cancer cell proliferation. In addition, in a mouse model, rosmarinic acid can significantly reduce the number of pulmonary metastatic tumor nodules by activating AMPK.

1.4 Antimicrobial effect
Rosmarinic acid has a certain inhibitory effect on bacteria. Rosmarinic acid 500 mmol/L can inhibit staphylococci, and the bacteriostatic activity is affected by pH and ion concentration [24]. Abedini et al. [25] found that rosmarinic acid 0.3-1.3 mg/mL has an inhibitory effect on Staphylococcus aureus 5001, Staphylococcus ludens T26A3, Klebsiella oxytoca, Enterococcus faecium C159-6, Pseudomonas aeruginosa ATCC27583, Corynebacterium, Mycobacterium smegmatis 5003 and Staphylococcus warneri T12A12. Rosemary acid inhibits Escherichia coli, Staphylococcus aureus, Salmonella and Bacillus subtilis by disrupting the cell structure and proteins of the bacteria and inhibiting their Na+,K+-ATPase activity, with varying degrees of inhibition depending on the bacteria [26].
In addition, rosmarinic acid also has antiviral effects. Under acidic conditions, rosmarinic acid reacts with nitrite ions to form 6-nitro and 6,6-dinitrorosmarinic acids [27]. These compounds can act as human immunodeficiency virus-1 integrase inhibitors at the micromolar level, inhibit viral replication in human T-cell leukemia MT-4 cells, and enhance anti-integrase inhibition and antiviral effects.
1.5 Other pharmacological effects
In addition to the above effects, rosmarinic acid also has neuroprotective, anti-angiogenic, and antidepressant effects. The neuroprotective and anti-angiogenic effects of rosmarinic acid are closely related to its antioxidant and anti-inflammatory properties. Ren et al. [28] confirmed in an in vitro neurotoxicity cell model experiment that the protective effect of rosmarinic acid is related to the reduction of reactive oxygen species production and mitochondrial function. Rosmarinic acid was found to have a neuroprotective effect in a rat model of Alzheimer's disease, possibly because it can prevent the antioxidant imbalance and cholinergic damage caused by β-amyloid [29].
Shang et al. [30] found that rosmarinic acid can reduce oxidative stress caused by spinal cord injury in mice, downregulate the inflammatory factor NF-κB and pro-inflammatory factors, thereby exerting neuroprotective effects. Huang et al. [31] selected human umbilical vein endothelial cells to study the anti-angiogenic effects and mechanisms of rosmarinic acid, and found that rosmarinic acid can dose-dependently inhibit angiogenesis processes including endothelial cell proliferation, migration, and tube formation, as well as reducing intracellular reactive oxygen species levels, vascular endothelial growth factor expression and IL-8 release. Mahmoud et al. [32] also demonstrated that rosmarinic acid enhances the therapeutic effect of paclitaxel on breast cancer by inhibiting angiogenesis. In addition, some studies have shown that rosmarinic acid has antidepressant effects. Lataliza et al. [33] studied the effect of rosmarinic acid on a mouse model of depression induced by lipopolysaccharide and found that rosmarinic acid exerts an antidepressant effect through the cannabinoid receptor/peroxisome proliferator-activated receptor γ signaling pathway. In addition, rosmarinic acid also has therapeutic effects on enteritis and gout, and has broad application prospects.
2 Application of rosemary acid delivery systems
As mentioned above, rosemary acid has various pharmacological effects such as anti-oxidation and anti-inflammation, and can be used to treat various diseases. However, the currently commonly used dosage forms are powders and solutions, which are difficult to meet the needs of different drug delivery routes and disease sites. Moreover, the shortcomings of the physical and chemical properties of rosemary acid itself also limit its clinical application [34]. To solve these problems, most researchers use new drug carriers to deliver rosmarinic acid to improve its therapeutic effect.
2.1 Nanodroplets
Nanodroplets are spontaneously formed emulsions of water, oil, surfactants and co-surfactants. They usually have a particle size of 1–100 nm and are thermodynamically stable, transparent or translucent homogeneous dispersions. They have the advantages of increasing the solubility of poorly soluble drugs, improving stability, reducing irritation and enhancing sustained release and targeted action [35]. Fachel et al. [36-37] prepared oil-in-water nanoemulsions of rosmarinic acid using the phospholipid self-emulsification method and response surface design method, and surface-modified them with chitosan to obtain chitosan-coated rosmarinic acid nanoemulsions. The results of nasal mucosal administration studies showed that the nanoemulsions had good adhesion, can delay drug release, have a long penetration time, and have a high drug penetration/retention rate in the nasal mucosa of pigs. In addition, the protective effect against nerve damage is better than that of the intraperitoneal injection route, which improves the bioavailability of rosmarinic acid in the brain. It has been further demonstrated that rosmarinic acid nanomilks can significantly reduce the proliferation of astrocytes and necrotic changes by reducing the production of reactive oxygen species and nitric oxide levels and preventing a decrease in total thiol content [38].
Marafon et al. [39] prepared rosemary acid nanomilks and evaluated the effect of topical application of a formulation containing the nonionic surfactant polysorbate 80. The results showed that polysorbate 80 had a positive effect on the retention/penetration of rosemary acid in full skin, and could be used in the development of topical applications for anti-aging skin care products. Panya et al. [40] studied the interaction between α-tocopherol and rosmarinic acid in emulsions and found that in O/W emulsions, rosmarinic acid and α-tocopherol exhibited strong synergistic effects, increasing the formation of caffeic acid and further improving the oxidative stability of the emulsion. Kittipongpittaya et al. [41] investigated the effect of pH on the antioxidant effect of rosemary acid and α-tocopherol in emulsions, and found that the synergistic antioxidant activity of the two was strongest at a pH of 7. In summary, rosemary acid can be used as a tool to study the interaction of antioxidants in emulsions.
Nanoemulsions are a type of nanoformulation. Their nanoscale particles and oil-water mixed systems can increase the solubility of drugs and avoid the first pass effect of the liver. Nanoemulsions of rosmarinic acid have certain advantages in nasal and transdermal administration. However, the low oil content of the nanoemulsions may lead to their low viscosity, and their retention at the mucosal administration site needs to be improved. In addition, the composition and stability of the nanoemulsion prescription are also issues that researchers need to focus on.
2.2 Lipid nanoparticles
Solid lipid nanoparticles (SLNs) are a nanoparticle drug delivery system made by adsorbing or encapsulating drugs in a lipid membrane using a solid natural or synthetic lipid with low toxicity, good biocompatibility and biodegradability as a carrier. It has good physicochemical stability, targeting, biocompatibility and the ability to regulate drug release [42].
Madureira et al. [43] used stearic acid and carnauba wax to prepare rosmarinic acid-loaded SLNs (RA SLNs) by hot melt ultrasonic method, and investigated the release of the two in the gastrointestinal tract. The results showed that the pH and enzymes of the digestive tract had a significant effect on RA SLNs. The zeta potential of the nanoparticles increased under simulated gastric conditions and decreased under simulated intestinal conditions. In particular, the particle size of the RA SLN prepared with carnauba wax increased significantly in the intestine. In experiments with human colorectal adenocarcinoma Caco-2 cells, the two types of SLN showed similar drug uptake.
However, in a mixed experiment using Caco-2 cells and human colon cancer HT29x cells, the drug uptake of the carnauba wax-based SLN was lower than that of the stearic acid-based SLN. Kuo et al. [44] used five solid lipid materials (beeswax, cocoa butter, glycerol dibehenate, glycerol tridecanoate, diphosphatidylglycerol) and the surfactants soy lecithin and polysorbate 80 to prepare W/O/W SLNs, and co-loaded them with nerve growth factor, rosmarinic acid, curcumin and quercetin. Then, the surface of the SLNs was modified with transferrin to increase targeting to blood-brain barrier cells.
The results showed that the nanoparticles could reduce the toxicity of the drug to blood-brain barrier cells, increase the targeting of blood-brain barrier cells, and reduce IL-6 secretion by inhibiting overexpressed caspase-3, extracellular signal-regulated kinase (ERK), p38 mitogen-activated protein kinase, reduce IL-6 secretion, enhance the expression of cAMP response element binding protein and phosphorylated ERK5, and improve antioxidant stress capacity. In addition, nanostructured lipid carriers (NLCs) are similar to SLNs, but the addition of liquid lipids to their formulations is more conducive to drug loading [42]. Chaiyana et al. [45] prepared NLC nanoparticles containing rosmarinic acid extract. These nanoparticles can control drug release, and their release and residence time in pig skin are superior to those of nanoemulsion formulations, making them an ideal formulation for dermal administration of rosmarinic acid.
Lipid nanoparticles use natural or synthetic lipid materials and have good biocompatibility, with different regulatory effects on drug release. Lipid nanoparticles of rosmarinic acid have shown good results in intravenous injection, intranasal administration, transdermal administration, and intestinal mucosal penetration. However, rosmarinic acid is not very hydrophobic, which may lead to problems such as burst release and low encapsulation rate of rosmarinic acid in lipid nanoparticles. Moreover, the limited types of lipids currently available cannot effectively resolve the conflict between the drug loading and sustained release properties. Therefore, the derivatization and modification of rosmarinic acid and the development of carrier materials with excellent properties will promote the development of its lipid nanoparticles.
2.3 Polymer micelles
Polymer micelles, also known as polymeric micelles, are mainly composed of amphiphilic copolymers that self-assemble in water to encapsulate poorly soluble drugs, forming a nano-structured micelle solution [46]. Arranz et al. [47] used protein micelles to encapsulate rosmarinic acid and evaluate the interaction between the carrier and functional ingredients. The results showed that the carrier had a significant effect on the drug encapsulation rate and could exert better biological functions, indicating the potential of protein carriers as rosmarinic acid drug carriers. In addition, rosmarinic acid can not only be used as an active pharmaceutical molecule, but also as part of the micelle carrier.
Chung et al. [48] used an amide reaction to combine the amino group of polyethylene glycol with the carboxyl group of rosmarinic acid to form a block copolymer. This block copolymer can self-assemble in a buffer to form polymer micelles with a particle size of (63.5±4.0) nm. Compared with intravenous injection of free drugs, the polymeric micelles of rosmarinic acid can better reduce colitis inflammation and inhibit the expression and production of pro-inflammatory factors than the intravenous injection of free drugs. In addition, the micelles can be used as drug carriers to deliver dexamethasone, which has been shown to have a synergistic therapeutic effect in a colitis model.
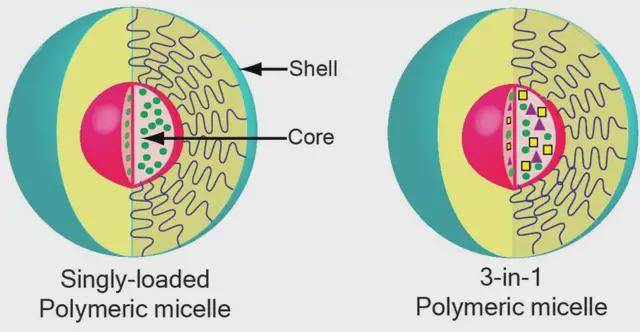
Liu et al. [49] linked rosmarinic acid to a highly sulfated poly(acrylic acid)-poly(ethylene glycol) polymer, which self-assembled into micelles to deliver tanshinone IIA. These micelles can effectively regulate the NF-κB pathway, reduce the expression of vascular cell adhesion molecule-1, inhibit inflammatory responses, reduce endothelial cell damage, and achieve synergistic treatment of atherosclerosis.
Polymer micelles have thermodynamic stability. The structure of the polymer can be adjusted by selecting the type and ratio of hydrophilic and hydrophobic blocks to optimize the drug-loading properties. Rosmarinic acid can not only be loaded into the interior of the polymer micelle, but also act as a carrier material to co-deliver other drugs for synergistic effects. In addition, polymer micelles can be modified with specific targeting molecules or introduced with environmentally sensitive bonds to achieve better therapeutic effects. However, the selection of polymeric carriers, in vivo degradation properties, in vivo stability, and the relationship between structure and properties restrict the development and utilization of polymeric micelles.
2.4 Polymeric micro/nanoparticles
Polymeric micro/nanoparticles based on biodegradable polymer materials are safe and non-toxic. They can encapsulate drugs within the structure and are promising drug carriers [50-51]. Chitosan has good biocompatibility, its structure is conducive to modification, and it has antioxidant and anti-inflammatory activities. It can be used to deliver rosmarinic acid to achieve synergistic effects. Da Silva et al. [52] used chitosan nanoparticles to protect the characteristics of bioactive antioxidants and prepare nanoparticles containing rosmarinic acid to achieve safe and innovative treatment.
Rosemary acid-loaded chitosan nanoparticles were prepared by a certain proportion of sodium tripolyphosphate ionic gelation method at pH 5.8, and were characterized by photonic correlation spectroscopy, scanning electron microscopy, high performance liquid chromatography and antioxidant activity. The results showed that the prepared nanoparticles were smooth spherical particles of about 300 nm in size, with a rosmarinic acid loading of up to 40%, and had good antioxidant activity. Eye delivery studies found that the nanoparticles were safe and non-toxic to human retinal epithelial ARPE-19 cells and human corneal epithelial HCE-T cells. The apparent permeation coefficients in the monolayer penetration experiments of HCE-T cells and IARPE-19 cells were (3.41±0.99)×10−5 and (3.39±0.18)×10−5, respectively, which is consistent with the characteristics of sustained-release drugs [53]. Casanova et al. [54] prepared rosemary acid chitosan particles with a particle size of 4–7 μm using spray drying, which can control the release rate of the drug for local delivery of rheumatoid arthritis. rosmarinic acid chitosan particles with a particle size of 4–7 μm, which can control the release rate of the drug for the local delivery of rheumatoid arthritis.
In addition, poly (D,L-lactic-co-glycolic acid) (PLGA) is one of the most commonly used biodegradable polymers, usually synthesized by ring-opening copolymerization of lactide and glycolide. García-Melero et al. [55] used PLGA as a carrier material to encapsulate rosmarinic acid and prepare nanoparticles with a diameter of 70–100 nm. These nanoparticles can control the slow release of the drug, have good free radical scavenging ability, do not affect cell proliferation activity, and can enhance cell uptake. The above results have laid a foundation for the application of rosemarinic acid nanoparticles in the biomedical field.
Polymer micro/nanoparticles are an ideal choice for the application of sustained and controlled release drug delivery. They can encapsulate drug molecules with different properties, protect drugs from degradation and changes in metabolic distribution in the body, and are easily administered through various routes. The polymeric microparticle delivery system of rosmarinic acid can regulate the controlled and sustained release curve of rosmarinic acid, improve permeability, and has wound healing, anti-inflammatory and neuroprotective effects. It can be used for ophthalmic, dermal, intravenous and other routes of administration. However, similar to polymer micelles, the types of polymer materials, functional modification methods, in vivo safety, and the interaction between the properties of drugs and polymer materials still require further research.
2.5 Grafted polymers
Natural polymers such as proteins and polysaccharides are biodegradable and biocompatible biomaterials that are widely used in drug delivery and tissue engineering [56]. Grafting reactive monomers or compounds onto polymers and its excellent properties can achieve better biological activity. Ge et al. [57] first coupled rosemary acid to a gelatin scaffold through a chemical reaction, then plasticized it with glycerin and crosslinked it with diallyl xanthan gum to prepare a rosemary acid-gelatin biodegradable membrane. The results showed that the membrane had good water resistance, strong mechanical properties and excellent UV blocking ability. The introduction of rosmarinic acid enhances the antioxidant and antibacterial activity of the gelatin film, which has broad application prospects in the fields of medicine and food packaging. Huerta-Madroñal et al. [58] synthesized novel water-soluble chitosan-rosmarinic acid conjugates (CSRA) by linking different amounts of rosmarinic acid to chitosan.

CSRA can scavenge free radicals, enhance antibacterial activity, and reduce UV-induced cell damage and reactive oxygen species production in fibroblasts and keratinocytes, and therefore has good potential for skin applications. In addition, based on the pharmacological activity of rosmarinic acid, Zhang et al. [59] synthesized a series of grafted polymers by linking chitosan or derivatives with rosmarinic acid or rosmarinic acid salt. All polymers significantly inhibited the production of nitric oxide and TNF-α induced by lipopolysaccharide in RAW264.7 cells, and were non-cytotoxic. The above results show that chitosan derivatives grafted with rosmarinic acid have good antioxidant and anti-inflammatory properties.
Grafted polymers are a unique drug delivery system that chemically links drugs to different polymer chains via chemical bonds or cross-linking agents. They have good stability, high drug loading capacity, and can also specifically control drug release. Researchers mainly link rosmarinic acid to polymers such as chitosan to enhance their anti-inflammatory and antibacterial effects. At present, there are only a limited number of chemical bonds or linkers commonly used in grafted polymers. The release, in vivo kinetics and action of drug molecules in different polymers and linkers have not been studied in depth, and comparative studies are generally lacking.
2.6 Liposomes
Liposomes are mainly composed of phospholipids and cholesterol. They are biocompatible, easily cross the membrane, and can carry both hydrophilic and lipophilic drugs. They are a drug carrier with great potential for application. Yücel et al. [60] prepared liposomes and nanosphere loaded with rosmarinic acid, with encapsulation rates of 55.6% and 43.4%, respectively. They had good stability and better antioxidant activity. A study of the transdermal application effectiveness of rosemary acid liposomes and liposomes found that liposomes can control the release of rosemary acid to a certain extent, and their stability decreases after being stored at different temperatures for 3 months. However, transdermal penetration and enzyme inhibition experiments found that liposomes containing rosemary acid are more effective than liposomes [61].
Baranauskaite et al. [62] encapsulated rosemary acid in liposomes to improve its solubility and stability. The dissolution behavior of the drug in the drug-loaded liposomes was determined using a pepsin-free artificial gastric juice basket method to verify its good stability. Subongkot et al. [63] developed fatty acid liposomes containing oleic acid, linoleic acid and linolenic acid to improve the skin penetration of rosemary acid. The prepared liposomes had a particle size of about 50 nm and a drug loading of 24.02%. The fatty acids could significantly promote the skin penetration of the drug-loaded liposomes. Laser confocal microscopy showed that the liposomes adhered to the skin and then released the encapsulated rosmarinic acid through the skin. This indicates that liposomes containing fatty acids can increase the transdermal efficiency of rosmarinic acid.
Liposomes are vesicles with a bilayer structure, in which hydrophobic drug molecules are encapsulated in the phospholipid bilayer. Lipid nanoparticles are solid or liquid lipids such as glyceryl monostearate and surfactants, and the drug is dispersed in the lipids. Therefore, liposomes are similar to lipid nanoparticles and also face the problems of low encapsulation rate, burst release and leakage. However, the bioactivity of rosemary acid liposomes is superior to that of free drugs, and they have good prospects for transdermal administration.
2.7 Other Carrier vehicles
Novel carrier delivery systems can improve the properties of drugs, facilitate drug administration, and improve stability and bioavailability. In addition to the delivery systems described above, cyclodextrin complexes, vesicles, phospholipid complexes, gels and polymeric implants have also been used for the delivery of rosmarinic acid [39,64-67]. Cyclodextrins can form complexes, non-complexes, conjugates and complexes with drugs, enhancing the stability and absorption of the drug. Rosmarinic acid is mainly inserted into the cavity of cyclodextrin in a 1:1 ratio to form a complex [64,68].
Fateminasab et al. [68] prepared complexes of rosmarinic acid with β-cyclodextrin and γ-cyclodextrin, and the solubility of rosmarinic acid increased linearly at 15–25 °C. In addition, the complexation of β-cyclodextrin and γ-cyclodextrin can significantly reduce the photosensitivity of rosmarinic acid to ultraviolet radiation, and has a long half-life (389.76–491.84 min). Antioxidant activity experiments have found that when rosmarinic acid is added to the cavity of cyclodextrin, the antioxidant activity decreases slightly within a certain drug concentration. It is speculated that the formation of the inclusion complex can mask some of the hydroxyl groups of rosmarinic acid. However, some studies have also shown that rosemary acid radical scavenging ability, copper reducing antioxidant capacity and oxygen radical absorption capacity can be enhanced by cyclodextrin complexation, which is related to the high water solubility of rosemary acid in the complex, the prevention of rapid oxidation and the formation of intramolecular hydrogen bonds [69-70].
In addition, Rodríguez-Luna et al. [71] loaded rosmarinic acid into a vehicle and then added it to carbomer to prepare a gel, and evaluated its anti-inflammatory activity in mice with psoriatic skin inflammation. The gel had a good protective effect on the oxidation index and antioxidant activity of rosmarinic acid, and significantly reduced levels of peritoneal edema, TNF-α and IL-6. Vieira et al. [67] developed a PLGA ophthalmic polymer implant loaded with rosmarinic acid for the treatment of neovascularization in the eye. The results showed that the rosmarinic acid implant was safe and released the drug continuously in the vitreous body for 6 weeks, which significantly reduced neovascularization, indicating its potential application in preventing neovascularization in ophthalmic diseases.
In summary, these delivery carrier systems can all improve the solubility, permeability, stability and bioavailability of rosmarinic acid, and promote its application potential. However, variables such as the composition and preparation method of the carrier can change the drug-loading characteristics of the drug delivery system and its in vitro and in vivo effects. At present, many studies have only been carried out in vitro, and there have been relatively few studies on in vivo effects, pharmacokinetics and in vivo tissue distribution.
3 Conclusion and outlook
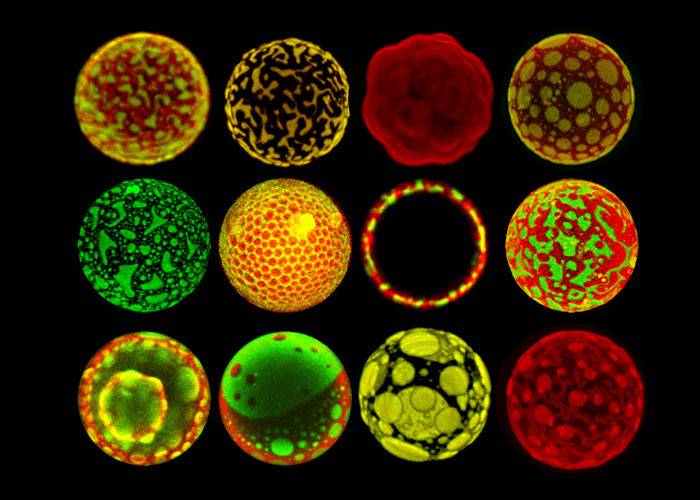
Currently, pharmaceutical researchers are increasingly focusing on the development of natural compounds with pharmacological activity. As mentioned earlier, rosmarinic acid can exert anti-inflammatory, antioxidant, and anti-tumor pharmacological effects through multiple mechanisms [72]. The representative mechanism of action is shown in Figure 2. It has become a new drug candidate with great development prospects [73-74].
The diverse pharmacological effects of rosmarinic acid can be used in different disease sites, but this also means that the existing simple dosage forms cannot fully utilize its effects. In addition, rosmarinic acid can be rapidly metabolized in vivo in different forms, including hydrolysis, methylation, sulfation, and glucuronidation [75]. However, the pharmacokinetic parameters reported in the literature vary, such as the time to peak [(0.19 ± 0.06), (1.08±0.38), (0.74±0.12) h] and maximum blood concentration [(1 087.64±572.72), (48.67±11.24), (37.19±13.85) ng/mL] [76-78]. The absolute oral bioavailability of rosmarinic acid is low, generally not exceeding 5% [76, 79], which may be related to gastrointestinal hydrolysis, poor permeability through the intestinal epithelial membrane, and the first-pass effect of the liver. Its apparent permeability coefficient of (0.20±0.05)×10−6 cm/s also indicates that rosmarinic acid has low permeability [80].
Drug delivery systems can enhance the solubility and permeability of rosmarinic acid, change the pharmacokinetic characteristics in vivo, and increase bioavailability. The maximum plasma concentration and area under the plasma concentration-time curve of the rosmarinic acid-loaded phospholipid complex (1063.299 ng/mL and 183569.927 ng·min/mL) were significantly higher than those of the free drug (327.068 ng/mL and 83670.936 ng·min/mL) [81], and the half-life and mean residence time of the polyethylene glycol nanoparticles also increased more than 4 times [46]. Current research mostly focuses on delivery vehicles such as emulsions, nanoparticles, micelles, liposomes, and cyclodextrin complexes. Although the ratio and prescription of these delivery systems can affect the properties of the preparation and the efficacy of the drug, the physicochemical properties and pharmacological activities of rosmarinic acid, such as its antioxidant, anti-inflammatory, and antibacterial activities, are significantly improved after being encapsulated by the drug carrier.
New dosage forms and structural derivatives of rosmarinic acid are aimed at improving bioavailability and reducing toxicity. At present, although many rosmarinic acid derivatives with better effects have been discovered in nature, these discoveries are often unpredictable [82]. In the future, targeted structural modification of rosmarinic acid should be carried out through in-depth research on its mechanism of action, and the influencing factors and different pharmacological effects of derivative drug delivery systems should be systematically investigated. In addition, most studies have mainly used conventional carrier systems such as complexes and emulsions to deliver rosmarinic acid for administration through different routes.
In the future, emphasis should be placed on designing controlled-release rosmarinic acid delivery systems that take into account the physiological environment of the disease site (e.g., increased reactive oxygen species at the site of inflammation) and the characteristics of different administration routes (e.g., the appropriate particle size for oral transmembrane absorption and pulmonary inhalation). At present, there is still a lack of in-depth research on the cellular level of action mechanisms and in vivo pharmacokinetic characteristics of rosemary acid delivery systems, such as cellular uptake and intracellular transport. In subsequent research, appropriate in vitro evaluation models and in vivo evaluation methods should be selected to improve the research basis for the mechanism of action and in vivo experiments of rosemary acid delivery systems, which is particularly important for the future development and utilization of rosemary acid.
Reference
[1]Petersen M, Simmonds M S J. Rosmarinic acid [J]. Phytochemistry, 2003, 62(2): 121-125.
[2]Deguchi Y, Ito M. Caffeic acid and rosmarinic acid contents in genus Perilla [J]. J Nat Med, 2020, 74(4): 834-839.
[3]Fachel F N S, Schuh R S, Veras K S, et al. An overview of the neuroprotective potential of rosmarinic acid and its association with nanotechnology-based delivery systems: A novel approach to treating neurodegenerative disorders[J]. NeurochemInt, 2019, 122: 47-58.
[4] Scarpati M L, Oriente G. Isolamento e costituzione dell’acido rosmarinico (dal rosmarinus off.) [J]. Ric Sci, 1958, 28: 2329-2333.
[5]Choi S H, Jang G W, Choi S I, et al. Development and validation of an analytical method for carnosol, carnosic acid and rosmarinic acid in food matrices and evaluation of the antioxidant activity of rosemary extract as a food additive [J]. Antioxidants, 2019, 8(3): 76.
[6]Matwiejczuk N, Galicka A, Zaręba I, et al. The protective effect of rosmarinic acid against unfavorable influence of methylparaben and propylparaben on collagen in human skin fibroblasts [J]. Nutrients, 2020, 12(5): 1282.
[7] Baek J, Lee M G. Oxidative stress and antioxidant strategies in dermatology [J]. Redox Rep, 2016, 21(4): 164-169.
[8]Chen Z C, Zhong C J. Oxidative stress in Alzheimer’s disease [J]. Neurosci Bull, 2014, 30(2): 271-281.
[9]Kirkham P A, Barnes P J. Oxidative stress in COPD [J]. Chest, 2013, 144(1): 266-273.
[10]deS Gil E, Enache T A, Oliveira-Brett A M. Redox behaviour of verbascoside and rosmarinic acid [J]. Comb Chem High Throughput Screen, 2013, 16(2): 92-97.
[11]Kim H J, Kim T H, Kang K C, et al. Microencapsulation of rosmarinic acid using polycaprolactone and various surfactants [J]. IntJ Cosmet Sci, 2010, 32(3): 185-191.
[12]Dahchour A. Anxiolytic and antidepressive potentials of rosmarinic acid: A review with a focus on antioxidant and anti-inflammatory effects [J]. Pharmacol Res, 2022, 184: 106421.
[13]Vostálová J, Zdařilová A, Svobodová A. Prunella vulgaris extract and rosmarinic acid prevent UVB-induced DNA damage and oxidative stress in HaCaT keratinocytes [J]. Arch Dermatol Res, 2010, 302(3): 171-181.
[14]Colica C, Di Renzo L, Aiello V, et al. Rosmarinic acid as potential anti-inflammatory agent [J]. Rev Recent Clin Trials, 2018, 13(4): 240-242.
[15]Scheckel K A, Degner S C, Romagnolo D F. Rosmarinic acid antagonizes activator protein-1-dependent activation of cyclooxygenase-2 expression in human cancer and nonmalignant cell lines [J]. J Nutr, 2008, 138(11): 2098-2105.
[16]Lembo S, Balato A, Di Caprio R, et al. The modulatory effect of ellagic acid and rosmarinic acid on ultraviolet-B-induced cytokine/chemokine gene expression in skin keratinocyte (HaCaT) cells [J]. Biomed ResInt, 2014, 2014: 346793.
[17]Rocha J, Eduardo-Figueira M, Barateiro A, et al.
Anti-inflammatory effect of rosmarinic acid and an extract of Rosmarinus officinalis in rat models of local and systemic inflammation [J]. Basic Clin Pharmacol Toxicol, 2015, 116(5): 398-413.
[18]Ghasemzadeh Rahbardar M, Amin B, Mehri S, et al. Anti-inflammatory effects of ethanolic extract of Rosmarinus officinalis L. and rosmarinic acid in a rat model of neuropathic pain [J]. Biomed Pharmacother, 2017, 86: 441-449.
[19]Cao W, Mo K, Wei S J, et al. Effects of rosmarinic acid on immunoregulatory activity and hepatocellular carcinoma cell apoptosis in H22 tumor-bearing mice [J]. Korean JPhysiolPharmacol, 2019, 23(6): 501-508.
[20] Li Hong, Zhuang Hailin, Lin Junjin, et al. Effects of rosmarinic acid components in swollen knotted wind on the proliferation, migration ability and expression of apoptosis-related genes in breast cancer cells [J]. Chinese Journal of Traditional Chinese Medicine, 2018, 43(16): 3335-3340.
[21]Karthikkumar V, Sivagami G, Vinothkumar R, et al. Modulatory efficacy of rosmarinic acid on premalignant lesions and antioxidant status in 1,2-dimethylhydrazine induced rat colon carcinogenesis [J]. Environ Toxicol Pharmacol, 2012, 34(3): 949-958.
[22] Saiko P, Steinmann M T, Schuster H, et al. Epigallocatechin gallate, ellagic acid, and rosmarinic acid perturb dNTP pools and inhibit de novo DNA synthesis and proliferation of human HL-60 promyelocytic leukemia cells: Synergism with Arabinofuranosylcytosine [J]. Phytomedicine, 2015, 22(1): 213-222.
[23]Han Y H, Kee J Y, Hong S H. Rosmarinic acid activates AMPK to inhibit metastasis of colorectal cancer [J]. Front Pharmacol, 2018, 9: 68.
[24]Suriyarak S, Gibis M, Schmidt H, et al. Antimicrobial mechanism and activity of dodecyl rosmarinate against Staphylococcus carnosus LTH1502 as influenced by addition of salt and change in pH [J]. J Food Prot, 2014, 77(3): 444-452.
[25]Abedini A, Roumy V, Mahieux S, et al. Rosmarinic acid and its methyl ester as antimicrobial components of the hydromethanolic extract of Hyptis atrorubens Poit. (Lamiaceae) [J]. Evid Based Complement Alternat Med, 2013, 2013: 604536.
[26]Zhang J H, Cui X, Zhang M, et al. The antibacterial mechanism of perilla rosmarinic acid [J]. BiotechnolAppl Biochem, 2022, 69(4): 1757-1764.
[27]Dubois M, Bailly F, Mbemba G, et al. Reaction of rosmarinic acid with nitrite ions in acidic conditions: Discovery of nitro- and dinitrorosmarinic acids as new anti-HIV-1 agents [J]. J Med Chem, 2008, 51(8): 2575-2579.[28]Ren P, Jiang H, Li R G, et al. Rosmarinic acid inhibits 6-OHDA-induced neurotoxicity by anti-oxidation in MES23.5 cells [J]. J Mol Neurosci, 2009, 39(1): 220-225.
[29] Gok D K, Hidisoglu E, Ocak G A, et al. Protective role of rosmarinic acid on amyloid beta 42-induced echoic memory decline: Implication of oxidative stress and cholinergic impairment [J]. Neurochem Int, 2018, 118: 1-13.
[30] Shang A J, Yang Y, Wang H Y, et al. Spinal cord injury effectively ameliorated by neuroprotective effects of rosmarinic acid [J]. Nutr Neurosci, 2017, 20(3): 172-179.
[31]Huang S S, Zheng R L. Rosmarinic acid inhibits angiogenesis and its mechanism of action in vitro [J]. Cancer Lett, 2006, 239(2): 271-280.
[32]Mahmoud M A, Okda T M, Omran G A, et al. Rosmarinic acid suppresses inflammation, angiogenesis, and improves paclitaxel induced apoptosis in a breast cancer model via NF3 κB-p53-Caspase-3 pathways modulation [J]. JAppl Biomed, 2021, 19(4): 202-209.
[33]Lataliza AAB, de Assis P M, da Rocha Laurindo L, et al. Antidepressant-like effect of rosmarinic acid during LPS-induced neuroinflammatory model: The potential role of cannabinoid receptors/PPAR-γ signaling pathway [J]. Phytother Res, 2021, 35(12): 6974-6989.
[34]Konishi Y, Kobayashi S. Transepithelial transport of rosmarinic acid in intestinal Caco-2 cell monolayers [J]. Biosci Biotechnol Biochem, 2005, 69(3): 583-591.
[35]Singh Y, Meher J G, Raval K, et al. Nanoemulsion: Concepts, development and applications in drug delivery [J]. J Control Release, 2017, 252: 28-49.
[36]Fachel F N S, Michels L R, Azambuja J H, et al. Chitosan-coated rosmarinic acid nanoemulsion nasal administration protects against LPS-induced memory deficit, neuroinflammation, and oxidative stress in Wistar rats [J]. NeurochemInt, 2020, 141: 104875.
[37]Fachel F N S, Medeiros-Neves B, Dal Prá M, et al. Box-Behnken design optimization of mucoadhesive chitosan-coated nanoemulsions for rosmarinic acid nasal delivery-in vitro studies [J]. Carbohydr Polym, 2018, 199: 572-582.
[38]Fachel F N S, Dal Prá M, Azambuja J H, et al. Glioprotective effect of chitosan-coated rosmarinic acid nanoemulsions against lipopolysaccharide-induced inflammation and oxidative stress in rat astrocyte primary cultures [J]. Cell Mol Neurobiol, 2020, 40(1): 123-139.
[39]Marafon P, Fachel F N S, Dal Prá M, et al. Development, physico-chemical characterization and in-vitro studies of hydrogels containing rosmarinic acid-loaded nanoemulsion
for topical application [J]. J Pharm Pharmacol, 2019, 71(8): 1199-1208.
[40]Panya A, Kittipongpittaya K, Laguerre M, et al. Interactions between α-tocopherol and rosmarinic acid and its alkyl esters in emulsions: Synergistic, additive, or antagonistic effect? [J]. J Agric Food Chem, 2012, 60(41): 10320-10330.
[41]Kittipongpittaya K, Panya A, Phonsatta N, et al. Effects of environmental pH on antioxidant interactions between rosmarinic acid and α-tocopherol in oil-in-water (O/W) emulsions [J]. J Agric Food Chem, 2016, 64(34): 6575-6583.
[42]Mirchandani Y, Patravale V B, Brijesh S. Solid lipid nanoparticles for hydrophilic drugs [J]. J Control Release, 2021, 335: 457-464.
[43]Madureira A R, Campos D A, Oliveira A, et al. Insights into the protective role of solid lipid nanoparticles on rosmarinic acid bioactivity during exposure to simulated gastrointestinal conditions [J]. Colloids Surf B Biointerfaces, 2016, 139: 277-284.
[44]Kuo Y C, Lou Y I, Rajesh R, et al. Multiple-component dual-phase solid lipid nanoparticles with conjugated transferrin for formulating antioxidants and nerve growth factor against neuronal apoptosis [J]. J Taiwan Inst Chem E, 2020, 110: 140-152.
[45]Chaiyana W, Anuchapreeda S, Somwongin S, et al. Dermal delivery enhancement of natural anti-ageing compounds from Ocimum sanctum Linn. extract by nanostructured lipid carriers [J]. Pharmaceutics, 2020, 12(4): 309.
[46]Cai Y, Qi J, Lu Y, et al. The in vivo fate of polymeric micelles [J]. Adv Drug Deliv Rev, 2022, 188: 114463.
[47]Arranz E, Villalva M, Guri A, et al. Protein matrices ensure safe and functional delivery of rosmarinic acid from marjoram (Origanum majorana) extracts [J]. J Sci Food Agric, 2019, 99(5): 2629-2635.
[48]Chung C H, Jung W, Keum H, et al. Nanoparticles derived from the natural antioxidant rosmarinic acid ameliorate acute inflammatory bowel disease [J]. ACS Nano, 2020, 14(6): 6887-6896.
[49]Liu M, Liu S, Zhu X, et al. Tanshinone IIA-loaded micelles functionalized with rosmarinic acid: A novel synergistic anti-inflammatory strategy for treatment of atherosclerosis [J]. JPharm Sci, 2022, 111(10): 2827-2838.
[50]Ding D W, Zhu Q D. Recent advances of PLGA micro/ nanoparticles for the delivery of biomacromolecular therapeutics [J]. Mater SciEng C, 2018, 92: 1041-1060.
[51]Karimi M, Ghasemi A, Sahandi Zangabad P, et al. Smart micro/nanoparticles in stimulus-responsive drug/gene delivery systems [J]. Chem Soc Rev, 2016, 45(5): 1457-1501.
[52]Da Silva S B, Amorim M, Fonte P, et al. Natural extracts into chitosan nanocarriers for rosmarinic acid drug delivery [J]. Pharm Biol, 2015, 53(5): 642-652.
[53]Da Silva S, Ferreira D, Pintado M, et al. Chitosan-based nanoparticles for rosmarinic acid ocular delivery-In vitro tests [J]. IntJ Biol Macromol, 2016, 84: 112-120.
[54]Casanova F, Estevinho B, Santos L. Preliminary studies of rosmarinic acid microencapsulation with chitosan and modified chitosan for topical delivery [J]. Powder Technol, 2016, 297: 44-49.
[55]García-Melero J, López-Mitjavila J J, García-Celma M J, et al. Rosmarinic acid-loaded polymeric nanoparticles prepared by low-energy nano-emulsion templating: Formulation, biophysical characterization, and in vitro studies [J]. Materials (Basel), 2022, 15(13): 4572.
[56]Rahimi M, Charmi G, Matyjaszewski K, et al. Recent developments in natural and synthetic polymeric drug delivery systems used for the treatment of osteoarthritis [J]. Acta Biomater, 2021, 123: 31-50.
[57]Ge L M, Zhu M J, Li X Y, et al. Development of active rosmarinic acid-gelatin biodegradable films with antioxidant and long-term antibacterial activities [J]. Food Hydrocoll, 2018, 83: 308-316.
[58]Huerta-Madroñal M, Caro-León J, Espinosa-Cano E, et al. Chitosan-rosmarinic acid conjugates with antioxidant, anti-inflammatory and photoprotective properties [J]. Carbohydr Polym, 2021, 273: 118619.
[59]Zhang J J, Wang L Q, Tan W Q, et al. Preparation of chitosan-rosmarinic acid derivatives with enhanced antioxidant and anti-inflammatory activities [J]. Carbohydr Polym, 2022, 296: 119943.
[60]Yücel Ç, Şeker Karatoprak G. Development and evaluation of the antioxidant activity of liposomes and nanospheres containing rosmarinic acid [J]. Farmacia, 2017, 65(1): 40-45.
[61]Yücel Ç, Şeker Karatoprak G, Değim İ T. Anti-aging formulation of rosmarinic acid-loaded ethosomes and liposomes [J]. J Microencapsul, 2019, 36(2): 180-191.
[62]Baranauskaite J, Duman G, Corapcıoğlu G, et al. Liposomal incorporation to improve dissolution and stability of rosmarinic acid and carvacrol extracted from oregano (O. onites L.) [J]. Biomed Res Int, 2018, 2018: 6147315.
[63] Subongkot T, Ngawhirunpat T, Opanasopit P. Development of ultradeformable liposomes with fatty
acids for enhanced dermal rosmarinic acid delivery [J]. Pharmaceutics, 2021, 13(3): 404.
[64]Aksamija A, Polidori A, Plasson R, et al. The inclusion complex of rosmarinic acid into beta-cyclodextrin: A thermodynamic and structural analysis by NMR and capillary electrophoresis [J]. Food Chem, 2016, 208: 258-263.
[65]Budhiraja A, Dhingra G. Development and characterization of a novel antiacne niosomal gel of rosmarinic acid [J]. Drug Deliv, 2015, 22(6): 723-730.
[66]Huang J H, Chen P X, Rogers M A, et al. Investigating the phospholipid effect on the bioaccessibility of rosmarinic acid-phospholipid complex through a dynamic gastrointestinal in vitro model [J]. Pharmaceutics, 2019, 11(4): 156.
[67]Vieira L C, Moreira C P S, Castro B F M, et al. Rosmarinic acid intravitreal implants: A new therapeutic approach for ocular neovascularization [J]. Planta Med, 2020, 86(17): 1286-1297.
[68]Fateminasab F, Bordbar A, Shityakov S, et al. Molecular insights into inclusion complex formation between β-and γ-cyclodextrins and rosmarinic acid [J]. J Mol Liq, 2020, 314: 113802.
[69]Veras K S, Fachel F N S, Delagustin M G, et al. Complexation of rosmarinic acid with hydroxypropyl-β-cyclodextrin and methyl-β-cyclodextrin: Formation of 2 ∶ 1 complexes with improved antioxidant activity [J]. J Mol Struct, 2019, 1195: 582-590.
[70]MedronhoB, Valente AJ M, Costa P, et al. M. Valente, A, Costa, P. Inclusion complexes of rosmarinic acid and cyclodextrins: Stoichiometry, association constants, and antioxidant potential [J]. Colloid Polym Sci, 2014, 292(4): 885-894.
[71]Rodríguez-Luna A, Talero E, Ávila-Román J, et al. Preparation and in vivo evaluation of rosmarinic acid-loaded transethosomes after percutaneous application on a psoriasis animal model [J]. AAPS Pharmscitech, 2021, 22(3): 103.
[72] Zhao Yuxia, Chen Yingqian. Rosemary acid alleviates ischemic brain injury in newborn rats through the AMPK/mTOR pathway [J]. Chinese Herbal Medicine, 2021, 52(22): 6897-6903.
[73]Atanasov A G, Zotchev S B, Dirsch V M, et al. Natural products in drug discovery: Advances and opportunities [J]. Nat Rev Drug Discov, 2021, 20(3): 200-216.
[74]Maher P. The potential of flavonoids for the treatment of neurodegenerative diseases [J]. Int J Mol Sci, 2019, 20(12): 3056.
[75] Guo Shaobo, Xu Lulu, Jiang Lijuan, et al. Analysis of the metabolites and metabolic pathways of rosmarinic acid in rats [J]. Chinese Journal of Traditional Chinese Medicine, 2019, 44(21): 4704-4712.
[76]Wang X Y, Qian Y X, Li X, et al. Rapid determination of rosmarinic acid and its two bioactive metabolites in the plasma of rats by LC-MS/MS and application to a pharmacokinetics study [J]. Biomed Chromatogr, 2021, 35(2): e4984.
[77]Ma B, Wang Y B, Zhang Q, et al. Simultaneous determination of oridonin, ponicidin and rosmarinic acid from Herba Isodi Rubescentis extract by LC-MS-MS in rat plasma [J]. J Chromatogr Sci, 2013, 51(10): 910-918.
[78]Liu Y, Li X, Li Y, et al. Simultaneous determination of danshensu, rosmarinic acid, cryptotanshinone, tanshinone IIA, tanshinone I and dihydrotanshinone I by liquid chromatographic-mass spectrometry and the application to pharmacokinetics in rats [J]. J Pharm Biomed Anal, 2010, 53(3): 698-704.
[79]Wang J X, Li G Y, Rui T Q, et al. Pharmacokinetics of rosmarinic acid in rats by LC-MS/MS: Absolute bioavailability and dose proportionality [J]. RSC Adv, 2017, 7(15): 9057-9063.
[80]Qiang Z, YeZ, Hauck C, et al. Permeability of rosmarinic acid in Prunella vulgaris and ursolic acid in Salvia officinalis extracts across Caco-2 cell monolayers [J]. J Ethnopharmacol, 2011, 137(3): 1107-1112.
[81]Yang J H, Zhang L, Li J S, et al. Enhanced oral bioavailability and prophylactic effects on oxidative stress and hepatic damage of an oil solution containing a rosmarinic acid-phospholipid complex [J]. J Funct Foods, 2015, 19: 63-73.
[82]Guan H Q, Luo W B, Bao B H, et al. A comprehensive review of rosmarinic acid: From phytochemistry to pharmacology and its new insight [J]. Molecules, 2022, 27(10): 3292.


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese






