What Is Hyaluronic Acid Made From?
Hyaluronic acid is also known as hyaluronic acid. It is a viscous polysaccharide composed of (1-3)-2-acetamido-2-deoxy-β-D-glucose units linked by β-1,4 and β-1,3 glycosidic bonds, alternately connected with (1-4)-O-β-D-glucuronic acid units. Hyaluronic acid is a widely distributed polysaccharide molecule in nature that forms a viscoelastic substance when combined with water. In the human body, it is primarily found in skin and connective tissues, serving as an extracellular matrix. In addition to providing cells with water and volume, it possesses properties such as tissue stability, strong binding capacity, high viscoelasticity, weak species and tissue specificity, and lack of immunogenicity. Hyaluronic acid has widespread applications in drug delivery, anti-adhesion in orthopaedic surgery, cardiology, arthritis, cancer therapy, ophthalmology, and food supplements.
1 Preparation of Hyaluronic Acid
1.1 Animal Tissue Extraction Method
In 1934, Meyer et al., professors of ophthalmology at Columbia University in the United States, first isolated this substance from the vitreous humour of cow eyes [1]. In the 1970s, Balazs et al. extracted hyaluronic acid from chicken combs and human umbilical cords [1].
The main process for extracting hyaluronic acid powder from animal tissues includes dehydration, grinding, soaking, extraction, purification, precipitation, and separation. The specific process is as follows: first, homogenise the tissue, then extract it with water and dilute salt solution. The extract is precipitated with chlorinated hexadecylpyridine or hexadecyl trimethylammonium bromide, The resulting precipitate is dissolved, the residue is removed, and the solution is precipitated with 2–3 times the volume of ethanol to obtain crude hyaluronic acid. Purification can be achieved by treating the crude product with ethanol or quaternary ammonium salts, or by further removing impurities and proteins using enzymatic hydrolysis, ultrafiltration, or ion exchange techniques, ultimately yielding the final product.

The tissue extraction method has the advantages of a simple process, high molecular weight, high viscosity, and strong moisturising properties. However, due to limitations in raw material availability and the coexistence of hyaluronic acid with other polysaccharides such as chondroitin sulfate in biological tissues, this method has low yield, poor separation, complex process, and high cost, making it unsuitable for large-scale production. It is more suitable for small-scale production with dispersed raw material sources. With the continuous increase in demand and application scope of hyaluronic acid, the animal tissue extraction method will inevitably be gradually replaced by other methods.
1.2 Microbial fermentation method
Since the 1970s, researchers have begun to utilise microbial fermentation to produce hyaluronic acid powder. Shiseido of Japan first reported the use of Streptococcus equi to produce hyaluronic acid in 1985. The commonly reported hyaluronic acid-producing bacteria are primarily the A and C groups of Streptococcus species listed in the Bergey's Manual. The A group mainly includes Streptococcus pyogenes, which are pathogenic to humans and unsuitable as production strains; the C group of Streptococcus species are non-pathogenic to humans and more suitable for industrial production. In recent years, foreign countries have already achieved industrial-scale production of hyaluronic acid using C group Streptococcus species [2].
Operational process: Inoculate the slant culture into conical flasks containing culture medium, incubate at 37°C for 12–16 hours, then transfer to seed tanks. The nitrogen source in the culture medium is peptone, beef extract, yeast extract, etc., the carbon source is glucose, and the inoculation ratio is 1:10. The fermentation broth formulation is essentially the same as the seed broth, except that the glucose content is higher, typically 3%–6%. Maintain an aeration rate of 0.3–1.0 vvm (volume of air per minute relative to the fermentation volume), stir at 120 rpm, and ferment at 37°C for 40–46 hours. During fermentation, adjust the pH to 6.5–7.0. In the later stages of fermentation, when the glucose concentration drops below 0.5% and the pH decreases slowly or stops decreasing, fermentation is complete. After fermentation, adjust the pH to 4.0–4.5 with trichloroacetic acid, filter to remove the bacterial mass, adjust the filtrate pH to 6.0–6.5, add 95% ethanol, and precipitate hyaluronic acid. Dissolve the precipitate in a 0.1 mol/L sodium chloride solution, stirring, add an excess of 1% CPC to form a complex precipitate with the hyaluronic acid in the filtrate, let stand, siphon off the mother liquor, wash the precipitate twice, dissolve in 0.4 mol/L sodium chloride solution with stirring overnight, filter, precipitate with ethanol, dehydrate with ethanol, and vacuum dry to obtain hyaluronic acid.
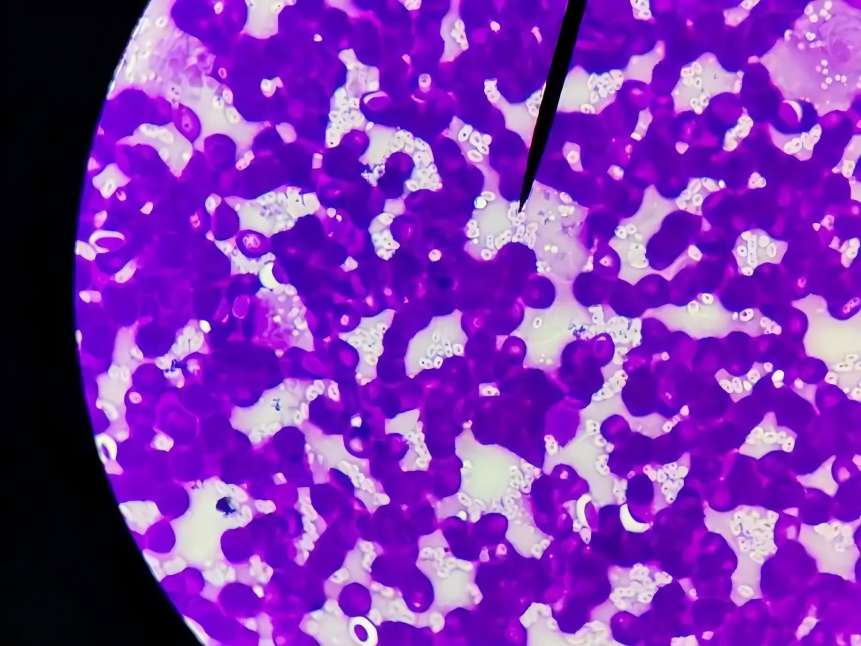
Currently, the fermentation method for producing hyaluronic acid as an alternative to tissue extraction has become a trend. The fermentation method for producing hyaluronic acid has a simple process, does not rely on animal tissues, and its yield is not limited by raw material sources. Additionally, hyaluronic acid exists in a free state in the fermentation broth, making it easy to separate, purify, and industrialise. Therefore, the fermentation method has become the primary method for industrial production of hyaluronic acid [3].
1.3 Artificial Synthesis Method
Related studies have shown that hyaluronic acid in living organisms is synthesised by hyaluronic acid synthase catalysing the reaction of UDP-G1cA and UDP-G1cNAc [4]. Therefore, researchers both domestically and internationally have attempted to synthesise hyaluronic acid in vitro using enzymatic methods and have made some progress. Neuman [5] reported a method for the artificial synthesis of hyaluronic acid, First, a polysaccharide polymer, one of the biological macromolecules, is used to synthesise hyaluronic acid oxazepane derivatives. Then, a decomposing enzyme (hyaluronidase from sheep or cow testes) is added to form a complex of the derivative and the enzyme. Finally, the enzyme is removed from the reaction solution, and hyaluronic acid is synthesised. Additionally, precipitation, separation, and purification are required.
Artificially synthesised hyaluronic acid is similar in quality to natural hyaluronic acid, but the precursor materials required for in vitro synthesis are expensive, so the artificial synthesis method is generally used for producing high-molecular-weight, high-purity hyaluronic acid [6].
2 Research on hyaluronic acid derivatives
Clinical applications have demonstrated that natural hyaluronic acid possesses excellent biocompatibility; however, it is easily degraded and diffused in tissues, resulting in short retention times in the body and suboptimal application outcomes. Recent studies have shown that hyaluronic acid derivatives obtained through modification and cross-linking can address these limitations [7].
The hydroxyl, carboxyl, N-acetylamino, and reducing ends of the hyaluronic acid molecule are the four sites susceptible to chemical modification, with primary modification methods including esterification, cross-linking, and grafting. The two most commonly used sites for covalent modification of hyaluronic acid are the carboxyl and hydroxyl groups. Currently reported derivatives with clinical application value are primarily new excipients derived from the modification of the hydroxyl and carboxyl groups of hyaluronic acid.
These derivatives can be selected based on their intended use, with appropriate cross-linking agents chosen to enhance relevant physical properties such as biocompatibility, degradability, in vivo retention time, drug loading capacity, and stability. Hyaluronic acid gels modified with diethyl sulfoxide (DVS) exhibit unique biocompatibility and other properties, solutions using aldehydes as cross-linking agents (hyaluronic acid fluids) exhibit high viscoelasticity, while cross-linking agents with multiple functional groups, such as epoxy compounds, can improve water solubility. Additionally, the reaction between cross-linking agents and the carboxyl groups of hyaluronic acid can produce derivatives, such as esters and amines, which enhance biocompatibility, among other properties [8]. Furthermore, cross-linking reactions can be used to design and prepare functional, intelligent drug carriers, thereby enhancing drug efficacy, improving drug targeting, and reducing adverse effects. Therefore, the use of cross-linking reactions to modify hyaluronic acid not only expands its application scope but also enhances its practical value [9].
3 Applications of Hyaluronic Acid Powder
3.1 Applications in Cosmetics
In the early 1980s, the excellent moisturising properties of hyaluronic acid garnered significant attention from the international cosmetics industry. Extensive literature and decades of domestic and international applications have demonstrated that hyaluronic acid can be used in cosmetics such as creams, lotions, masks, beauty serums, toners, lipsticks, foundations, and essences, as well as in products like shampoos, conditioners, mousses, and facial cleansers. For example, Restylane by Swiss company Restylane, Hydrobella moisturising lotion by French company Maybelline, and domestic brands such as Yongfang, Ziranmei, and Lvdanlan [10]. In cosmetics, hyaluronic acid plays a role in moisturising, preventing and repairing skin damage, nourishing and lubricating the skin, and having antibacterial and anti-inflammatory effects. Currently, for the rejuvenation of facial wrinkles, botulinum toxin and skin fillers are the two main non-surgical treatment methods, targeting dynamic and static wrinkles, respectively. Since hyaluronic acid was first used as a skin filler, its advantages and efficacy have gradually gained recognition from both medical professionals and patients, leading to a steady increase in usage. It has broken the dominance of collagen-based products and has ranked first in usage in the United States for five consecutive years [11].

3.2 Applications in Food
In China, over 98% of hyaluronic acid is primarily used in the pharmaceutical, clinical diagnosis, and cosmetics industries. Hyaluronic acid is still in its infancy in the food sector, with limited reports available. In fact, hyaluronic acid is not only used topically for moisturisation; oral hyaluronic acid can also enhance the body's hydration. Through digestion and absorption, hyaluronic acid can enhance vitality and youthfulness; it can moisturise and smooth the skin, making it soft and elastic; and it can delay aging and prevent conditions such as arthritis, arteriosclerosis, arrhythmia, and cerebral atrophy. An increasing number of hyaluronic acid-based beauty and health supplements are available both domestically and internationally, such as Hyaron ECM·E produced by the Japanese Hyaluronic Acid Research Institute, Beauty Fast capsules produced by Natural-Max, Hyaluronic Acid capsules and tablets produced by Source Naturals, and domestically available oral beauty collagen hyaluronic acid and Rui'er Water Source capsules.
3.3 Clinical Applications
Pure hyaluronic acid formulations are available in three forms for clinical use: liquid spray, gel application, and film coverage. Hyaluronic acid is widely used in ophthalmology and orthopaedics and has expanded into many other fields, including general surgery, otolaryngology, and hand surgery. Hyaluronic acid is used to treat bone and joint diseases, effectively alleviating arthritis, joint pain, and regulating joint function. It has also shown good results in fracture fixation surgery, joint stiffness, and lumbar discectomy injection therapy. Postoperative tissue adhesion is a major challenge in surgery. Extensive clinical trials have demonstrated that hyaluronic acid effectively prevents postoperative adhesion, significantly reducing complications and sequelae caused by adhesion. Since hyaluronic acid is a natural component of human and animal bodies, it is safe and reliable as a pharmaceutical raw material with no side effects. Therefore, hyaluronic acid is a highly popular new biomaterial in the medical field today.
Pang Suqiu et al. [12] used hyaluronic acid solution to treat dry eye syndrome, and clinical results indicated that hyaluronic acid has a good therapeutic effect on dry eye disease. Goto et al. [13] administered sodium hyaluronate into the joint cavities of 25 patients with chronic progressive joint diseases, and followed up with clinical symptoms and parameters. The results showed significant improvements in all indicators, with patients' conditions improving. Luo Hongtu et al. [14] randomly divided 396 patients undergoing various thyroid surgeries into two groups. The experimental group (214 cases) received hyaluronic acid injections on the thyroid wound surface, deep to the anterior neck muscle group, the deep layer of the platysma muscle. The control group of 182 patients did not receive hyaluronic acid.

The results showed that 26 cases of postoperative adhesion occurred in the experimental group, while 41 cases occurred in the control group, with a significant difference between the two groups. Additionally, hyaluronic acid, as an important component of the extracellular matrix, regulates interactions between cells and between cells and the matrix, promoting wound healing and inhibiting abnormal scar formation caused by excessive collagen deposition. Hyaluronic acid also promotes granulation tissue formation, reduces scab area, shortens scab detachment time, and has a promoting effect on burn healing. Jiang Lixia et al. [8] reported that spraying burn patients with hyaluronic acid artificial skin powder resulted in good therapeutic effects and high safety.
3.4 Applications in Pharmacy
3.4.1 Improving Drug Stability
Freeze-dried single-chamber liposomes tend to reform into large multi-chamber liposomes, which is detrimental to therapies requiring small particle liposomes. Wang Yuhui [15] reported that by bonding sodium hyaluronic acid to the surface of biodegradable liposomes via hydrogen bonds, the transformation of freeze-dried single-chamber liposomes into large multi-chamber liposomes could be effectively inhibited, thereby stabilising freeze-dried single-chamber liposomes. Peer et al. [16] prepared hyaluronic acid-heparin conjugate gels and bound recombinant human basic fibroblast growth factor-2 (FGF-2) to the heparin end of the hyaluronic acid-heparin conjugate. In vitro analyses indicated that hyaluronic acid-heparin conjugate gels enhance the stability and activity of FGF-2.
3.4.2 Applications in controlled-release formulations
Hyaluronic acid and its derivatives can serve as sustained-release carriers for various drugs, such as anticancer drugs, anti-inflammatory drugs, and anaesthetics. Hyaluronic acid has diverse application forms as a drug carrier. Chou et al. [17] prepared hyaluronic acid-coated polycyanoacrylate butyl ester nanoparticles (hyaluronic acid-PBCA), which were obtained through a free radical polymerisation reaction of hyaluronic acid monomers and polycyanoacrylate monomers. Using paclitaxel as a model anticancer drug, the encapsulation efficiency of hyaluronic acid-PBCA nanoparticles reached 90%. The tumor cell proliferation inhibitory effect of paclitaxel-loaded hyaluronic acid-PBCA nanoparticles was significantly higher than that of paclitaxel-loaded PBCA nanoparticles and paclitaxel injection. Homma et al. [18] conjugated hyaluronic acid with the anti-inflammatory drug methotrexate using short peptides and linkers to form hyaluronic acid-methotrexate conjugates for the treatment of osteoarthritis, achieving controlled-release of the drug at the site of inflammation and effectively reducing the toxic side effects of methotrexate. Hyaluronic acid hn et al. [19] prepared injectable hyaluronic acid microgel for the controlled release of erythropoietin (EPO). In vivo release experiments showed that EPO was slowly released from the microgel, with plasma EPO concentrations exceeding 0.1 mg/L, which is the minimum concentration required for EPO to exert its effects. This concentration was maintained for 7 days without significant toxic side effects.

Hyaluronic acid and its derivatives as carriers offer unique biocompatibility, rheological properties, and chemical and physical diversity, making them an effective sustained-release system for pharmacologically active molecules. The practical application of hyaluronic acid as a biological carrier combined with various drugs will be a key focus of future research and development.
3.4.3 Application in Anticancer Drugs
Research has shown that certain solid tumours and metastatic lymphocytes express high levels of hyaluronic acid receptors—CD44—with which hyaluronic acid has a strong affinity. As a targeted carrier for antitumour drugs, hyaluronic acid can bind smaller drug molecules to its network structure or graft drug molecules onto hyaluronic acid-based drug carriers, targeted binding with receptors on the surface of tumour cells, enabling more drug molecules to enter tumour tissue, increasing the absorption and retention time of anticancer drugs in tumours and lymph nodes, thereby enhancing drug efficacy and reducing toxic side effects. Luo et al. [20] esterified hyaluronic acid with paclitaxel to form a bio-targeted prodrug. Fluorescent labelling revealed that the drug could specifically bind to cells, and this binding could be blocked by excess hyaluronic acid and anti-CD44 antibodies but not by chondroitin sulfate. Paclitaxel was released through the hydrolysis of the ester bond. Brown et al. [21] administered 5-fluorouracil and methotrexine containing hyaluronic acid and without hyaluronic acid to nude mice with thymoma via tail vein injection, The results showed that the drug concentrations in the tumour tissue increased by 403% and 106%, respectively.
Hyaluronic acid and its derivatives can be formulated into drug compositions or used as carriers to target and retain different drugs in various parts of the human body. This not only enables drugs to act on more precise target sites, increasing the concentration of therapeutic drugs at the site of action and significantly enhancing therapeutic efficacy, but also avoids drug side effects, providing a more effective approach for disease treatment [22].
3.5 Biomaterials
As a biomaterial, hyaluronic acid possesses advantages such as good biocompatibility and rapid biodegradability. Chen Jianying et al. [23] conducted biocompatibility tests on cross-linked hyaluronic acid gel membranes (CIIA-gel) in terms of in vitro haemolysis, cytotoxicity, acute toxicity, eye irritation, intradermal reaction, sensitisation, and genotoxicity. The results demonstrated that CIIA-gel material exhibits excellent biocompatibility and stable physical and chemical properties. Xiao Rongdong et al. [24] conducted in vivo degradation tests on hyaluronic acid membranes, which conformed to the general process of biodegradation of biomaterials in vivo, with no significant inflammatory reactions and satisfactory tissue compatibility. Fan Hongbin, Hu Yunyu et al. [25] conducted experimental studies on gelatin-chondroitin sulfate-sodium hyaluronate as a tissue engineering cartilage scaffold, demonstrated that gelatin-chondroitin sulfate-sodium hyaluronate porous scaffolds prepared by vacuum drying at 80°C exhibit good pore size, porosity, and compressive load-bearing capacity, and show good compatibility with rabbit bone marrow mesenchymal stem cells (MSCs), making them a novel biomimetic scaffold material for cartilage tissue engineering.
4 Analysis and Summary
In recent years, hyaluronic acid has developed rapidly. In 1985, the total global sales of hyaluronic acid in the international market reached 100 million USD, rising to over 200 million USD in 1990. By 2004, the global market size for hyaluronic acid applications was approximately 3 billion USD, and by 2012, it had grown to approximately 4.5 billion USD. Statistical data show that in 2012, the total sales of hyaluronic acid as a single skin filler in the international market reached 1.4 billion US dollars, with the markets for drug cosmetics and skincare products and medical products each accounting for half [26-28].
As a new type of excipient, hyaluronic acid has advantages such as good biocompatibility, rapid degradation, excellent moisturising properties, and tissue stability. However, several issues still hinder the development of hyaluronic acid in China. First, China's production capacity for hyaluronic acid is far from meeting market demand, especially for high-molecular-weight pharmaceutical-grade hyaluronic acid, which must be imported from abroad. Therefore, increasing the molecular weight and production volume of hyaluronic acid is an urgent issue to address.

Second, the variety of hyaluronic acid derivatives is relatively limited, with similar physical and chemical properties, limiting the range of options available and necessitating further research and development. Third, there are no clear grading standards for hyaluronic acid, which is currently classified into food-grade, cosmetic-grade, and pharmaceutical-grade categories based on intended use. The criteria for these classifications are vague, and there is significant overlap between grades, causing significant inconvenience in practical applications. Fourth, when used as a drug carrier, there is no standard method for calculating drug loading capacity, which affects drug content and preparation processes. Fifth, the process of combining hyaluronic acid with other materials to produce biomaterials is still immature, with low production rates and currently at an early stage, requiring further research.
Additionally, the yield and quality of hyaluronic acid produced by microbial methods primarily depend on the following factors: the performance of the production strain, the culture medium, the optimisation of fermentation processes, and the control of fermentation and subsequent separation and purification [29-30]. In China, due to limitations in fermentation equipment, processes, and strain selection, the production level and efficiency of hyaluronic acid are relatively low compared to foreign countries, with imports being the primary source, especially for high-purity, high-molecular-weight hyaluronic acid. Due to these limitations, the price of hyaluronic acid in China remains high. However, with the increasing maturity of fermentation technology in China, growing health awareness, and improved understanding of hyaluronic acid, the market for food-grade hyaluronic acid has seen rapid expansion in recent years. In summary, whether for pharmaceutical, cosmetic, or food applications, hyaluronic acid holds vast development potential and demand.
Finally, it is hoped that through the joint efforts of domestic and international scholars, more innovative ideas and applications can be applied to hyaluronic acid research and development, ensuring that the comprehensive development of hyaluronic acid is just around the corner.
References
[1] Bai Huiyu, Xu Jing, Li Huijun, et al. Research Progress on the Preparation and Application of Hyaluronic Acid [J]. Guangdong Chemical Industry, 2010, 37(11): 332.
[2] Song Lei, Wang Tengfei. A Review of the Current Status of Hyaluronic Acid Research [J]. Journal of Shandong Light Industry College, 2012, 26(2): 78.
[3] Chen Yihan, Ye Rui, Qian Yue, et al. Research Progress on the Biochemical Production of Hyaluronic Acid [J]. Journal of Shanghai Institute of Applied Technology, 2012, 12(2): 1124.
[4] Valarie L, Bruce A. Purification and lipid dependence of the recombinant hyaluronan synthases from Streptococcus pyogenes and Streptococcus equisimilis [J]. J Biol Chem, 1999, 274(7):4239.
[5] Neuman MG, Orua L, Coto G, et al. Hyaluronic acid signals for repair in ethanol-induced apoptosis in skin cells in vitro [J]. Clin Biochem, 2010, 43 (10/11): 822.
[6] Ozgenel G, Et6z A. Effects of repetitive injections of hyaluronic acid on peritendinous adhesions after flexor tendon repair: a preliminary randomised, placebo-controlled clinical trial [J]. Ulus Travma Acil Cerrahi Derg, 2012, 18(1): 11.
[7] Balazs E A, Laurent T C. Round table discussion: new applications for hyaluronan [A]. Laurent T C. The chemistry, biology, and medical application of hyaluronan and its derivatives [M]. London: Portland Press, 1998: 325.
[8] Jiang Lixia, Wang Wenbin. Applications of hyaluronic acid and its derivatives in medicine [J]. Chinese Journal of Reconstructive Surgery, 2010, 14(15): 56.
[9] Xu Xin, Shi Danping, Ye Wenxi, et al. Progress in the preparation of cross-linked hyaluronan derivatives [J]. Guangdong Chemical Industry, 2012, 39(5): 99.
[10] Pan Hongmei. A review of the current status of hyaluronan research [J]. Sichuan Food and Fermentation, 2003, 1(8): 67.
[11] Wu Sufan. Basic knowledge and clinical applications of hyaluronic acid [J]. Modern Practical Medicine, 2010, 22(4): 171.
[12] Pang Suqiu, Zhou Jinsheng, Chen Qiushuang, et al. Clinical applications of sodium hyaluronate [J]. Straits Pharmacy, 2011, 15(4): 252.
[13] Goto M, Hanyu T, Yoshio T, et al. Intra-articular injection of hyaluronate (SI-6601D) improves joint pain and synovial fluid prostaglandin E2 levels in rheumatoid arthritis: a multicenter clinical trial [J]. Clin Exp Rheumatol, 2001, 19(4): 377.
[14] Luo Hongtu, Yang Shao Yu. Study on the preventive effect of sodium hyaluronate on postoperative adhesions after thyroid surgery [J]. Journal of Clinical Surgery, 2009, 12(5): 313.
[15] Wang Yuhui. Application of hyaluronic acid and its sodium salts in pharmaceutical formulations [J]. Food and Medicine, 2011, 7(8): 78.
[16] Yang Hao, Xiong Wenshuo, Ying Guoqing, et al. Preparation and application of cross-linked hyaluronic acid derivatives [J]. Chemical Industry Progress, 2006, 5(9): 234.
[17] Chou W Y, Ko J Y, Wang FS, et al. Effect of sodium hyaluronate treatment on rotator cuff lesions without complete tears: a randomised, double-blind, placebo-controlled study [J]. Journal of Shoulder and Elbow Surgery, 2010, 19(4): 557.
[18] Homm A, Sato H, Tamura T, et al. Synthesis and optimisation of hyaluronic acid-methotrexate conjugates to maximise benefit in the treatment of osteoarthritis [J]. Bioorganic & Medicinal Chemistry, 2010, 18(3): 1062.
[19]Hahn S, Kim JS, Shimoboujit H. Injectable hyaluronic acid microhydrogels for controlled release formulation of erythropoietin [J]. J Biomed Mater Res A, 2007, 80(4): 916.
[20]Luo Y, Ziebell M R, Prestwich G D. A hyaluronic acid-taxol antitumor bioconjugate targeted to cancer cells [J]. Biomacromolecules, 2000, 1(2): 208.
[21]Brown T J, Hatherell E M, Falzon J L, et al. Hyaluronan targeting of anti-metabolite anti-cancer drugs to human breast tumour xenografts [Z]. (2005) Submitted to Cancer Chemother Pharmacol.
[22] Liu Z, Wang B. New advances in the clinical research of hyaluronic acid [J]. Food and Medicine, 2006, 8(12): 98.
[23] Chen Jianying, Song Haibo. Preparation and biocompatibility study of cross-linked hyaluronan gel membranes [J]. Biomedical Engineering Research, 2009, 28(2): 104.
[24] Xiao Rongdong, Weng Guoxing. Comparison of mechanical properties and tissue compatibility of collagen/hyaluronan membranes and gelatin sponge scaffold materials [J]. Chinese Journal of Tissue Engineering Research, 2012, 16(25): 1123.
[25] Fan Hongbin, Yun Yu. Experimental study on gelatin-chondroitin sulphate-sodium hyaluronate as a tissue engineering cartilage scaffold [J]. Chinese Journal of Reconstructive Surgery, 2005, 19(6): 473.
[26] Chou CL, Li HW, Lee SH, et al. Effect of intra-articular injection of hyaluronic acid in rheumatoid arthritis patients with knee osteoarthritis [J]. Journal of the Chinese Medical Association, 2008, 71(8): 411.
[27]Lee H, Lee K, Park TG. Hyaluronic acid-paclitaxel conjugate micelles: synthesis, characterisation, and antitumour activity [J]. Bioconjugate Chemistry, 2008, 19(6): 1319.
[28]Benjamin Y S O, Ranganath S H, Lee L Y, et al. Paclitaxel delivery from PLGA foams for controlled release in post-surgical chemotherapy against glioblastoma multiforme [J]. Biomaterial, 2009, 30(12): 3189.
[29]Park K, Lee M Y, Kim K S, et al. Target-specific tumour treatment by VEGF siRNA complexed with reducible polyethyleneimine hyaluronic acid conjugate [J]. Biomaterials, 2010, 31(19): 5258.
[30]Sudhir H, Yilong F, Davis Y, et al. The use of submicro nano-scale PLGA implants to deliver paclitaxel with enhanced pharmacokinetics and therapeutic efficacy in intracranial glioma in mice [J]. Biomaterial, 2010, 31(3): 5199.


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese








