What Are the Uses of Hyaluronic Acid Powder in Osteoarthritis?
Hyaluronic acid was first isolated from the vitreous humour of cow eyes by Meyer and Palmer in 1934. It is a high-molecular-weight polysaccharide composed of glucuronic acid and N-acetylglucosamine as its disaccharide units, widely distributed in animal tissue cells, and constitutes various matrices within the body. Over the past 20 years, hyaluronic acid and its derivatives have been extensively used in ophthalmology, otolaryngology, orthopaedics, and general surgery, yielding satisfactory results.
1 Application of hyaluronic acid in the treatment of osteoarthritis in the elderly
Hyaluronic acid powder has been used to treat osteoarthritis for over 40 years. Endre and Balazs first proposed the concept of viscoelastic supplementation therapy for osteoarthritis in the 1960s. They found that when humans and horses suffer from osteoarthritis, the viscoelasticity and shock-absorbing capacity of their joint synovial fluid are significantly lower than those of normal joints, leading to reduced protective and lubricating functions. Viscosupplementation therapy involves replenishing viscoelastic substances to restore the fluid dynamics of normal joint synovial fluid, thereby promoting the regeneration and function of normal tissue [1]. Over the past 20 years, intra-articular injection of high-viscosity hyaluronic acid for the treatment of knee osteoarthritis has been widely applied in clinical practice. Numerous literature reports exist on this topic, but conclusions vary. Wobig et al. [2] and Patrella et al. [3] independently employed randomised double-blind methods to compare the efficacy of hyaluronic acid and saline in treating osteoarthritis, yielding diametrically opposed results.
Wobig found that the pain relief rate in weight-bearing activities was 39%–56% in the hyaluronic acid group at follow-up after 10–24 weeks, while only 13% in the saline group. In contrast, Petrella evaluated 120 patients using the WOMAC score, VAS score, and functional improvement assessment, and found that the efficacy of the hyaluronic acid group and the saline group was similar, with no significant differences. Petrella [4] recently analysed the results of a randomised double-blind clinical study involving 106 patients and found that intra-articular injection of hyaluronic acid compared with placebo showed significant differences in WOMAC scores and SF-36 scores, The authors further divided the hyaluronic acid treatment group into a 3-injection group and a 6-injection group, and found no significant differences in efficacy between the two groups. Sun et al. [5] conducted a prospective study using a healthy population aged 50 years as a control group to investigate the outcomes of hyaluronic acid treatment for unilateral knee osteoarthritis in the elderly. Follow-up at 6 months revealed that patients who received intra-articular hyaluronic acid injections experienced improvements in pain symptoms, knee joint function, and balance, with effects observable as early as one week and sustained for six months.
Clinically, mucolytic therapy is commonly used for mild osteoarthritis, but this method is rarely applied to moderate to severe patients. Yavuzer et al. [6] attempted this approach, treating 20 patients with Kellgren and Lawrence grade II or III osteoarthritis using cross-linked hyaluronic acid (Hylan G-F 20). with an average age of (63.2 ± 4.4) years. At 1 week post-treatment, the WOMAC score decreased from 42.1 ± 15.2 to 37.9 ± 13.5. Additionally, the authors were the first to analyse the effects of hyaluronic acid intra-articular injection on gait improvement in patients with osteoarthritis. The results showed that after intra-articular injection of Hy-lan G-F20, the patients exhibited improved knee gait during walking, reduced valgus range of motion, and significantly enhanced weight-bearing capacity. Barrett et al. [7] conducted a retrospective analysis of 248 patients with moderate to severe osteoarthritis treated with hyaluronic acid therapy, finding that 60.1% achieved clinical success, as these patients avoided total knee arthroplasty or other clinical interventions following mucopolysaccharide supplementation therapy.
In addition to the above reports, recent scholars have conducted a comprehensive analysis of previous literature on hyaluronic acid powder therapy for osteoarthritis. Theiler et al. [1] analysed 63 randomised controlled clinical trials and concluded that viscoelastic supplementation therapy demonstrated positive effects on pain relief, functional recovery, and patient self-assessment in knee osteoarthritis, with pain relief rates ranging from 11% to 54% and functional recovery rates from 9% to 15%. Wang et al. [8] analysed literature from the MEDLINE and EMBASE databases from 1966 to 2001 on hyaluronic acid treatment for osteoarthritis, confirming that different types of hyaluronic acid preparations, whether cross-linked or non-cross-linked, administered via intra-articular injection, can alleviate osteoarthritis symptoms, significantly relieve pain, and improve knee joint function, making it a safe and effective treatment option.

However, some studies have questioned the efficacy of hyaluronic acid viscoelastic supplementation for osteoarthritis, arguing that this treatment is costly and cannot halt the progression of the disease. Arrich et al. [9] analysed literature from several databases on hyaluronic acid treatment for osteoarthritis and concluded that hyaluronic acid does not improve joint function in osteoarthritis, only alleviating pain after activity, with no effect on rest pain.
Viscoelastic supplementation therapy is widely accepted in clinical practice for early-stage osteoarthritis patients who have not previously undergone hyaluronic acid treatment. However, there is uncertainty regarding whether to continue with viscosupplementation or opt for surgical intervention when pain symptoms recur after initial treatment. Petrel-la [10] administered intra-articular hyaluronic acid injections to 537 patients with osteoarthritis who experienced recurrent pain and functional limitations after their first hyaluronic acid treatment. The results confirmed that clinical symptoms could also be improved, with potentially more pronounced effects, and without increasing the incidence of side effects.
The molecular weight of hyaluronic acid commonly used in clinical practice is typically 500–2500 kDa, with a treatment course consisting of 3–5 consecutive weeks of injections. Depending on the specific hyaluronic acid formulation, there may be variations. Generally, low-molecular-weight hyaluronic acid is administered in a course of 5 injections (e.g., Shipeite), while high-molecular-weight hyaluronic acid derived from cross-linked hyaluronic acid derivatives is administered in three sessions per course (e.g., Xinwei Ke) [1]. Some researchers [11] treated 246 patients with knee osteoarthritis using the same hyaluronic acid formulation, administering three injections or five injections per treatment course via intra-articular injection. The efficacy was evaluated using the Lasholm score, and no significant differences were observed at 5 weeks and 3 months post-treatment. Other researchers compared the efficacy of high-molecular-weight hyaluronic acid and low-molecular-weight hyaluronic acid in the treatment of osteoarthritis. Oron et al. [12] divided 522 patients into two groups and treated them with hyaluronic acid of molecular weights 1.55 and 6 × 10⁶ Dal, respectively. The results showed no significant differences in VAS scores at 3, 6, and 12 months of follow-up between the two groups, suggesting that hyaluronic acid with different molecular weights has no significant difference in alleviating pain symptoms in osteoarthritis.
Regarding the adverse effects associated with intra-articular injection of hyaluronic acid, other researchers have also conducted relevant statistical analyses. Kemper et al. [13] analysed the incidence of adverse effects in 4,253 patients following intra-articular injection of hyaluronic acid, finding that 180 cases (4.2%) experienced injection-related adverse effects. The most common adverse effects were: joint effusion (2.4%), joint swelling (1.3%), joint pain (1.2%), local joint warmth (0.6%), and injection site erythema (0.3%). Most of these side effects were mild to moderate, accounting for 21.4% and 40.3%, respectively, confirming that intra-articular injection of hyaluronic acid is a treatment option that patients can tolerate.
Clinical applications have revealed that some hyaluronic acid products may induce immune antigenic reactions in humans. Goomer et al. [14] investigated the immune antigenic reactions of natural hyaluronic acid and synthetic hyaluronic acid, finding that synthetic hyaluronic acid can cause delayed hypersensitivity reactions, while natural hyaluronic acid did not exhibit hypersensitivity reactions. Wang et al. [8] also found, based on an analysis of previous literature, that some patients who received injections of high-molecular-weight cross-linked hyaluronic acid (Hylan G-F 20) experienced knee pain and swelling, with an incidence rate of 7% to 20%. Whether these reactions are related to the residual protein and bacterial endotoxin content in synthetic hyaluronic acid requires further investigation.
2 Mechanism of action of hyaluronic acid in the treatment of osteoarthritis in the elderly
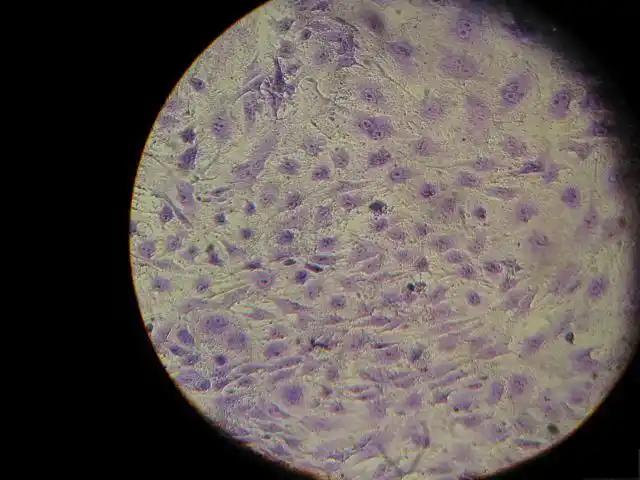
2.1 Interaction between hyaluronic acid and the cartilage cell surface receptor CD44
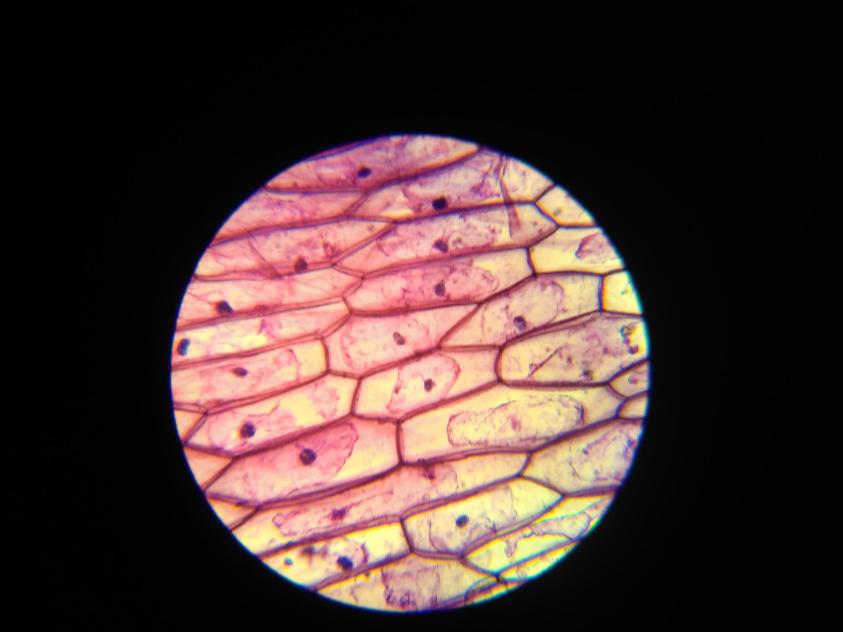
Hyaluronic acid plays a crucial role in maintaining the viscoelastic properties of synovial fluid. In patients with osteoarthritis, the concentration and molecular weight of hyaluronic acid in the knee joint are significantly reduced, leading to impaired viscoelastic protective function. Therefore, some researchers have attempted to use hyaluronic acid for synovial fluid supplementation therapy to treat osteoarthritis, believing it can provide viscoelasticity and lubrication. Clinical applications have confirmed that intra-articular injection of hyaluronic acid helps improve joint lubrication, which is beyond doubt. However, studies have found that after being injected into the joint cavity, hyaluronic acid has a very short metabolic half-life (12–17 hours), while its clinical efficacy can persist for several months (average 6 months). The short metabolic cycle of hyaluronic acid cannot fully explain the long-term efficacy observed in clinical settings. Therefore, it is considered that hyaluronic acid merely plays a mechanical lubricating role is incomplete. Recent studies have shown that chondrocytes have CD44 glycoproteins on their cell membranes, which are hyaluronic acid receptors. Exogenous hyaluronic acid can bind to the CD44 receptors on chondrocytes to exert direct biological effects, thereby exerting additional effects on chondrocytes in vivo, which explains the mechanism of its long-term effects [15,16].
The binding of hyaluronic acid powder to the CD44 receptors on chondrocytes helps stabilise the tissue microenvironment, influencing chondrocytes' response to cytokines and cell survival rates, thereby promoting tissue reconstruction. The presence of cartilage matrix influences the binding and dissociation of soluble morphogenetic factors with signal receptors, and may simultaneously establish a new or decoupled cell-matrix interaction, altering cellular response to morphogenetic factors [17].
Myazaki et al. [18] proposed that hyaluronic acid can bind to the CD44 receptor on the cell surface via fibronectin, thereby enhancing mitotic activity. Aruffo et al. [19] further investigated the effect of hyaluronic acid on cell generation and found that when the concentration of hyaluronic acid in the matrix increased, the cells' ability to synthesise hyaluronic acid significantly accelerated, suggesting that hyaluronic acid exerts a positive feedback regulatory mechanism on cell synthesis. Akmal et al. [15] also found that isolated chondrocytes exhibit a concentration-dependent response to hyaluronic acid when studying its effects on metabolic activity. However, contrary to Aruffo's view, Akmal proposed that the interaction between hyaluronic acid and CD44 is negative feedback, with cartilage cell proliferation and cartilage matrix product levels increasing as hyaluronic acid concentration decreases.
2.2 Effects of hyaluronic acid on nitric oxide production and cartilage cell apoptosis in joint cartilage
Research suggests that nitric oxide has a significant damaging effect on articular cartilage and may be an important factor in cartilage damage in osteoarthritis. It has been demonstrated that the synthesis of nitric oxide in osteoarthritis patients is directly correlated with the extent of cartilage damage, and inhibiting nitric oxide synthesis can slow down cartilage degeneration. Nitric oxide can also induce programmed cell death in chondrocytes, and osteoarthritic cartilage contains more apoptotic cells than normal tissue [20]. Blanco et al. [21] suggested that programmed cell death of chondrocytes is a predisposing factor for osteoarthritis. Therefore, studies have investigated the effects of hyaluronic acid on nitric oxide production and chondrocyte apoptosis in joint cartilage. Díaz-Gallego et al. [20] treated animals with osteoarthritis induced by anterior cruciate ligament transection with hyaluronic acid, then measured chondrocyte apoptosis and nitric oxide production levels. The results showed that hyaluronic acid could inhibit chondrocyte apoptosis, with a chondrocyte apoptosis rate of 9.81% in the treatment group, significantly lower than the 14.09% in the untreated group. Nitric oxide production was also significantly reduced, consistent with the findings of Moreland [22].

2.3 Other studies on the effects of hyaluronic acid in the treatment of osteoarthritis in the elderly
In addition to the above studies, other researchers have explored the mechanisms of hyaluronic acid's effects on joint cartilage from different angles. Larsen et al. [23] cultured 35S-labelled cartilage slices and induced chondrocyte damage with oxygen free radicals. and found that co-administration of a high-viscosity hyaluronic acid solution protected chondrocytes from oxygen free radical damage. It was speculated that this might be due to hyaluronic acid interacting with the cellular matrix, aggregating on the surface of chondrocytes, stabilising the cellular matrix, and forming a molecular barrier to block oxygen free radicals from damaging chondrocytes. Studies have confirmed that exogenous hyaluronic acid can stimulate human synovial cells to secrete hyaluronic acid in vitro, stimulate the synthesis of endogenous hyaluronic acid, inhibit its degradation, and simultaneously stimulate proteoglycan synthesis. Additionally, studies have confirmed that after hyaluronic acid injection, the content of chondroitin sulfate in joint synovial fluid significantly decreased, and chondroitin sulfate is a marker of cartilage tissue degradation [24].
Wang et al. [25] administered high-molecular-weight hyaluronic acid via intra-articular injection to 15 patients with knee osteoarthritis, then extracted synovial fluid for analysis of the expression of cytokines and enzymes associated with osteoarthritis. The results showed that high-molecular-weight hyaluronic acid reduced the gene expression of interleukin-8, tumour necrosis factor-α, and nitric oxide synthase, which may also be one of the mechanisms by which hyaluronic acid treats osteoarthritis in the elderly.
3 Conclusions
In summary, hyaluronic acid powder has a certain therapeutic effect on osteoarthritis, but its clinical efficacy remains controversial. The mechanism of action of hyaluronic acid on osteoarthritis requires further investigation.
Reference
[1]Theiler R ,Bruhlmann P.Overall tolerability and anal- gesic activity of intra-articular sodium hyaluronate in the treatment of knee osteoarthritis.Cur Med Res Opin ,2005,21:1727-1733.
[2]Wobig M ,Dickhut A ,Maier R ,et al.Visco supple- mentation with Hylan G-F20:a 26-week controlled trial of efficacy and safety in the osteoarthritic knee. Clin T her ,1998,20:410-423.
[3]Pat rella RJ ,DiSilvestro MD ,Hildebrand C.Effects of hyaluronate sodium on pain and physical functioning in osteoarthritis of the knee:a randomized ,double-blind , placebo controlled clinical trial.Arch Intern Med , 2002,162:292-298.
[4]Petrella RJ ,Petrella M.A prospective ,randomized , double-blind ,placebo controlled study to evaluate the efficacy of intraarticular hyaluronic acid for o steoar- thritis of the knee.J Rheumatol ,2006,33:951-956.
[5]Sun SF ,Hsu CW ,Hwang CW.Hyaluronate improves pain ,physical function and balance in the geriatric os- teoarthritic knee: a 6-month follow -up study using clinical tests.Osteoarthritis Cartilage ,2006,14:696- 701.
[6]Yavuzer G ,Sonel B ,Suldur N ,et al.Effects of intra- articular Hylan G-F 20injections on clinical and biome- chanical characteristics of the knee in osteoarthritis. Int J Rehabilit Res ,2005,28:371-374.
[7]Barrett JP ,Siviero P.Retrospective study of outcomes in hyalgan-treated patients with osteoarthritis of the knee.Clin Drug Invest ,2002,23:87-97.
[8]Wang CT ,Lin J ,Chang CJ ,et al.Therapeutic effects of hyaluronic acid on osteoarthritis of the knee:a met - analysis of randomized controlled trials.J Bone Joint Surg Am ,2004,86:538-545.
[9]Arrich J ,Piribauer F ,Mad P ,et al.Intra-articular hy - aluronic acid for the treatment of osteoarthritis of the knee:systematic review and meta-analysis .Can Med J ,2005,172:1039-1043.
[10]Petrella RJ.Hyaluronic acid for the treatment of knee osteoarthritis long-term outcomes from a naturalistic primary care experience. Am J Phy s Med Rehabil , 2005,84:278-283.
[11] Wang Jian-guo, Zheng Yuxin, Shi Yinyu. Clinical analysis of sodium hyaluronate in the treatment of knee osteoarthritis. Chinese Drugs and Clinical, 2004, 4: 580-582.
[12] Oron A , Mirovsky Y , Agar G ,et al. Viscosup- plementation in treatment of knee osteoarthritis: findings from clinical practice in Israel.J Bone Jt Surg Br Vol ,2005,87-B:388.
[13]Kemper F ,Gebhardt U ,Meng T ,et al.T olerability and short-term effectiveness of Hylan G-F 20in 4253 patients with osteoarthritis of the knee in clinical practice.Curr Med Res Opin ,2005,21:1261-1269.
[14]Goomer RS ,Leslie K ,Maris T ,et al.Native hyalu- ronan produces less hypersensitivity than cross-linked hyaluronan.Clin Orthop Relat Res ,2005,434:239- 245.
[15]Akmal M ,Singh A ,Anand A ,et al.The effects of hyaluronic acid on articular cho ndrocytes.J Bone Jt Surg Br Vol ,2005,87-B:1143-1149.
[16]Knudson W ,Casey B ,Nishida Y ,et al.Hyaluronan oligo saccharides perturb cartilage matrix homeostasis and induce cho ndrocytic cho ndroly sis. Arthritis Rheum ,2000,43:1165-1174.
[17] Knudson CB ,Knudson W. Hyaluronan and CD44 modulators of cho ndrocyte metabolism.Clin Orthop R ,2004,427S:S152-S162.
[18] Myazaki T , Myauchi S ,Nakamura T ,et al .The effect of sodium hyaluro nate on the growth of rabbit corneal epithelial cells in v itro.J Ocul Pharmacol T - her ,1996,12:409-415.
[19]Aruffo A ,Stamenkovic I ,Mlnick M ,et al.CD44is the principal cell surface receptor for hyaluronate. Cell ,1990,61:1303-1313.
[20]Díaz-Gallego L ,Prieto J ,Coronel P ,et al.Apoptosis and nitric oxide in an experimental model of o steoar- thritis in rabbit after hyaluronic acid treatment.J Or- thop Res ,2005,23:1370-1377.
[21] Blanco FJ , Guitian R , Vázquez-Mart ul E ,et al.Cho ndrocytes OA die by apoptosis:a possible explanation for ethiopathogenesis of OA. Arthritis Rheum ,1998,38:540-545.
[22]Moreland LW.Intra-articular hyaluronan(hyaluronic acid)and hylans for the treatment of osteoarthritis: mechanism of action.Arthritis Res T her ,2003,5:54- 67.
[23]Larsen NE ,Lombard KM ,Parenet EG.Effects of hy - aluronan on cartilage and cho ndrocyte culture.J Or- thop Res ,1992,10:23-32.
[24]Khanuja HS ,Hungerford MW ,Manjoo A.Intraar- ticular injections for the treatment of osteoarthritis of the knee: basic science , results , and indications. Curr Opin Orthop ,2003,14:62-68.
[25]Wang CT ,Lin YT ,Chiang BL ,et al.High molecular weight hyaluronic acid dow n-regulates the gene expression of osteoarthritis-associated cytokines and en- zymes in fibroblast-like synoviocytes from patients with early osteoarthritis. Osteoarthritis Cartilage , 2006,14:1237-1247.


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese







