What Is the Use of Nano Curcumin?
Curcumin (Cur) is a natural polyphenolic drug extracted from the rhizome of the plant turmeric [1]. Curcumin has a wide range of biological activities and has long been used to treat many diseases. In cancer therapy, curcumin inhibits oxidative stress, reduces lipid peroxidation and DNA single-strand breaks, inhibits cyclooxygenase (COX-1, COX-2) and NF-κB activation, and has an anti-proliferative effect. In addition, it induces apoptosis by targeting mitochondria and affects the signaling of the p53 tumor protein [2].
Curcumin's specific molecular targets have therapeutic implications in cancer signaling pathways [3]. Curcumin also effectively inhibits the production of reactive oxygen species (ROS) and reactive nitrogen species (RNS) in the cell environment. Curcumin also lowers low-density lipoprotein (LDL), inhibits oxidation of proteins and DNA. In Alzheimer's disease (AD), curcumin protects against β-amyloid (Aβ)-induced oxidative stress, prevents the formation and extension of Aβ fibrils, destabilizes Aβ fibrils, inhibits acetylcholinesterase, reduces neuroinflammation, and chelates transition metals [4]. During angiogenesis, curcumin can inhibit and downregulate the expression of various pro-angiogenic factors [5].
Despite the promising applications of curcumin, its limitations such as poor water solubility, low stability, low bioavailability, poor permeability and poor targeting have reduced its use as a therapeutic drug. Nanocarriers can significantly reduce the side effects of drugs by increasing their water solubility, thereby reducing the required dosage [6]. Functionalization of the surface of nanoparticles can increase ligand recognition for specific targeting. Nano-based formulations such as liposomes, micelles, polymeric nanomaterials and magnetic nanoparticles can coat and protect curcumin from degradation, improve bioavailability and deliver it efficiently to target cells [7-8]. The introduction of nanotechnology has the potential to enhance the therapeutic activity of this natural drug by improving its water dispersibility and cellular uptake. Therefore, the encapsulation of curcumin in nanoparticles will help to improve the solubility and circulation time of curcumin in the body, improving its biomedical applications.
1 Curcumin nanocarriers
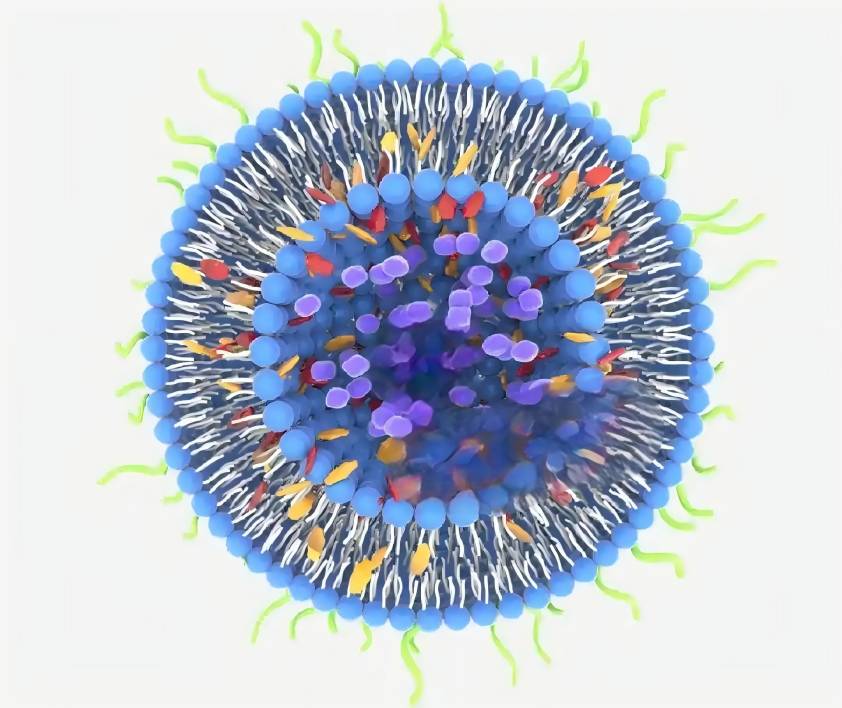
1.1 Liposomes
Liposomes are self-assembled spherical vesicles with a phospholipid bilayer [9-11]. They can effectively incorporate lipophilic compounds such as curcumin into their phospholipid bilayer structure, enhancing their cellular uptake while protecting the drug from light and chemical degradation [12]. Liposomes have a composition similar to biological cell membranes, so they have advantages as targeted drug carriers. Due to their non-toxicity, non-immunogenicity, variable drug loading and ease of preparation, various liposomal formulations have been developed [13]. The incorporation of nanoliposomes is beneficial for the application of curcumin, as it can improve the solubility, biological activity and bioavailability of curcumin, and maintain stability under adverse conditions. CHEN [14] et al. used cholesterol, Tween 80 and phospholipids to incorporate curcumin into nanoliposomes, which had a good effect on the storage stability and solubility of curcumin. Under alkaline pH conditions, the nano-liposome system can reduce its degradation rate.
1.2 Solid lipid nanoparticles
Solid lipid nanoparticles (SLNs) are a type of drug delivery system composed of biodegradable solid lipids, with the drug encapsulated or embedded in a lipid core composed of a high-melting-point fat matrix [15-16]. SLNs are a new type of carrier system with a wide range of applications. They have the advantages of good stability, high bioavailability, good sustained release and good dispersion when preparing lipophilic bioactive substances such as curcumin [17]. Curcumin was incorporated into SLNs by microemulsification technology. After 12 months of storage at 5 °C, the particle size and encapsulation efficiency of the nanostructured particles remained unchanged [18]. Rahman [19] and others prepared Cur-SLNs using high-speed homogenization. This drug delivery system has good stability. After 12 months of storage at 30 °C, there was no significant difference in the average size, encapsulation efficiency, and loading capacity.
1.3 Polymeric nanoparticles
Polymer nanoparticles are popular due to their many advantages, such as improving the therapeutic index of drugs by limiting their toxicity, protecting them from degradation in vivo and in vitro, altering their distribution, clearance and other pharmacokinetic parameters or controlling their release. Their polymeric matrix can encapsulate active pharmaceutical ingredients (APIs) with high encapsulation efficiency and stability. Another advantage is its drug targeting and adaptability to various drug delivery routes (including oral, nasal and non-intestinal routes) [20-23]. TSAI [24] et al. used high-pressure emulsification/solvent evaporation to incorporate curcumin into PLGA nanoparticles. The particle size of this preparation was 163 nm, and the encapsulation rate was 46.9%. Compared with free curcumin, this nanoparticle increased the oral bioavailability of curcumin by 22 times, and the residence time of curcumin in the cerebral cortex and hippocampus increased by 96% and 83%, respectively.
1.4 Nanogels
Nanogels are usually formed by physical self-assembly or chemical cross-linking of amphiphilic or hydrophilic polymer networks. The preparation of nanogels combines the advantages of hydrogels and nanoparticles, with high drug loading, biocompatibility and drug release responsiveness, making them ideal drug delivery materials. In addition, the large surface area and the presence of functional groups in nanogels can be further modified to target formulations or other biomolecules [25]. In one study, curcumin was coupled to cholesterol hyaluronan (CHA) nanogels for targeted delivery to CD44-expressing cancer cells [26], significantly downregulating the expression of COX-2, TNF-α and NF-κB.
1.5 Polymeric micelles
Polymer micelles are composed of amphiphilic copolymers in aqueous solution, with hydrophilic layers such as polyethylene glycol and polyvinyl alcohol, and a hydrophobic internal part such as biodegradable polyester and polyamino acids. Polymer micelles are stable and can encapsulate hydrophobic compounds such as curcumin to protect it from degradation and improve its circulation time and targeting to the desired cells [27-28]. Experimental studies of a curcumin-loaded TPGS/F127/P123 mixed polymeric micelle for the treatment of cervical cancer showed that the system had greater stability and sustained release after 6 days compared to free curcumin, and had selective targeting to NIH3T3 cancer cells [29].
2 Application of curcumin nanocarriers
2.1 Cancer
Curcumin has anticancer effects on many malignant tumors, but its poor pharmacokinetic properties limit its clinical efficacy [30]. Nanocarriers can improve the pharmacokinetic properties of curcumin, such as higher bioavailability and longer biological half-life, as well as increase drug delivery to specific sites, enhance its anticancer effect, It can also protect curcumin from degradation, increase its solubility, control drug release, promote membrane transport and absorption, and enhance cellular uptake [31]. BAEK [32] and others prepared stable N-carboxymethylchitosan-coated curcumin-loaded nanoparticles, which had higher cellular uptake and cytotoxicity against MCF-7 cells. Compared with a free curcumin suspension, lymphatic uptake and oral bioavailability of this nanoparticle formulation were 6.3 and 9.5 times higher, respectively. GONG [33] et al. evaluated the efficacy of curcumin-loaded polymeric micelles against lung cancer. Compared with free curcumin, curcumin nanoparticles had sustained in vitro release characteristics, in vitro anti-angiogenesis, enhanced cell uptake and cytotoxicity. In subcutaneous and pulmonary metastatic LL/2 tumor models, the micelles also showed significant antitumor efficacy compared to the free form.
2.2 Eye diseases
DAVIS [34] et al. prepared Pluronic-F127-stabilized D-α-tocopherol polyethylene glycol 1000 succinate nanoparticles. The study found that this nanocarrier significantly protected against cobalt chloride-induced hypoxia and glutamate-induced toxicity in vitro, and improved the viability of R28 cells. In an in vivo model of glaucoma-related high intraocular pressure and partial optic nerve transection, the formulation significantly reduced the loss of retinal ganglion cells compared to the control group. LI [35] et al. used a polyvinyl caprolactam-polyvinyl alcohol-polyethylene glycol (PVCL-PVA-PEG) graft copolymer to prepare a new type of curcumin nanomicelle, which significantly improved its solubility, chemical stability and antioxidant activity after encapsulation.
Compared with the free curcumin, the nanomicelle showed a higher solubility, chemical stability and antioxidant activity, and a lower toxicity. In an in vivo model of glaucoma-related high intraocular pressure and partial optic nerve transection, the formulation significantly reduced the loss of retinal ganglion cells compared to the control group. LI [35] et al. used a polyvinyl caprolactam-polyvinyl alcohol-polyethylene glycol (PVCL-PVA-PEG) graft copolymer to prepare glycol (PVCL-PVA-PEG) graft copolymer to prepare a new curcumin nanomicelle, which significantly improves its solubility, chemical stability and antioxidant activity after encapsulation. Compared with the free curcumin solution, this nanomedicine significantly improves cell uptake in vitro and corneal permeability in vivo, and improves anti-inflammatory efficacy.
2.3 Antibacterial
Curcumin is a traditional antimicrobial drug, and its antibacterial effect can be improved by combining it with different nanoparticles. XIE [36] et al. prepared curcumin nanoparticles using supercritical CO2. This nanodrug has higher solubility and enhanced antibacterial, antioxidant and anticancer effects. and its minimum inhibitory concentration (MIC) was 50% lower than that of free curcumin solution. VIMALA [37] et al. studied the antibacterial wound/burn dressing of curcumin wrapped in a chitosan-PVA-silver nanocomposite film, and found that it had a significant inhibitory effect on the growth of Escherichia coli compared with natural curcumin or chitosan-PVA-silver nanofilm.
2.4 Antiviral
Curcumin is a natural compound with antiviral properties that can directly interfere with viral replication mechanisms or inhibit the inflammatory response and apoptosis of cells in the viral replication cycle. Its signal pathways include PI3K/Akt and NF-κB [38]. GANDAPU [39] and others studied the potential of curcumin-loaded transferrin iron-transporting nanoparticle to inhibit human immunodeficiency virus (HIV-1) replication in vitro. Compared to free curcumin, the nanoparticles can deliver curcumin continuously and reduce its cytotoxicity by 50%. Curcumin nanoparticles have 3 times higher anti-HIV activity than their free form, can inhibit the expression of IL-1β, Topo II α and COX-2 induced by HIV-1, and block the synthesis of viral cDNA. YANG [40] et al. introduced curcumin-modified silver nanoparticles (AgNPs) to enhance the synergistic antiviral effect of curcumin and AgNPs in respiratory syncytial virus (RSV) infection. In tissue culture infection dose assays, the nanoparticles showed a high inhibitory effect on RSV infection, with a 2-fold decrease in viral titer, which inactivated RSV and prevented infection of host cells.
2.5 Wound healing
Curcumin can promote the wound healing process through various mechanisms, including its involvement in tissue remodeling processes, granulation or tissue formation, collagen deposition, and its ability to interfere with epithelial cell regeneration, promote fibroblast proliferation and vascular density [41-42]. LI [43] et al. prepared a curcumin nanoparticle using methoxypolyethylene glycol-b-poly (ɛ-caprolactone) copolymer (MPEG-PCL) which were incorporated into N,O-carboxymethyl chitosan/oxidized alginate hydrogels. This nanodelivery system showed improved stability and sustained release, and in vivo wound healing experiments showed improved re-epithelialization and collagen deposition in damaged tissue.
3 Conclusion
Curcumin is a natural compound with polyphenolic properties. This bioactive ingredient has a wide range of functions. Curcumin offers a new platform for the treatment of various diseases and has broad application prospects. Despite its multi-target potential in vitro, its pharmacological effects in vivo are limited due to its low water solubility, rapid metabolism and rapid clearance. Therefore, the particle size can be reduced by nanotechnology, the surface can be modified, and curcumin can be encapsulated with different nanocarriers to improve its bioavailability and biological activity.

This paper reviews the research progress of curcumin nanocarriers in recent years. Nanoparticles can significantly improve the in vitro and in vivo efficacy of curcumin and play a role in the prevention and treatment of various diseases. In addition, curcumin nanocarriers can reduce the dose of major therapeutic drugs, thereby improving efficacy and reducing toxicity. Although many curcumin-encapsulating nanocarriers have solved many delivery problems, further in vivo studies and safety evaluations of clinical trials are needed to optimize the delivery system, as well as studies on the chemical stability and degradation kinetics of curcumin nanosystems to promote their safe use in patients.
References:
[1] Liu W, Gu XZ, Wu XN, et al. Research progress on the pharmacological effects of curcumin [J]. West China Journal of Pharmacy, 2021, 36(3): 336-340.
[2] Zhang JH, Zhang Y, Lin XY, et al. Curcumin regulates p53 protein nuclear import to induce apoptosis in myeloma cells [J]. Journal of Applied and Environmental Biology, 2019, 25(4): 892-896.
[3] Wang Zexia, Feng Ye, Liu Fei, et al. Research progress on curcumin targeted therapy for cancer [J]. Journal of Hubei University of Science and Technology (Medical Sciences), 2019, 33(1): 86-89.
[4]SHEN L , JI H F . The pharmacology of curcumin: is it the degradation products?[J]. Trends in Molecular Medicine, 2012, 18(3):138-144.
[5] Li YQ, Li XJ. Basic and clinical research progress on the antitumor effect of curcumin [J]. Chinese Journal of Pharmacology and Toxicology, 2020, 34(5): 321-335.
[6] FARJADIAN F , MOGHOOFEI M , MIRKIANI S , et al. Bacterial components as naturally inspired nano-carriers for drug/gene delivery and immunization: Set the bugs to work?[J]. Biotechnology Advances, 2018 ,36(4):968-985.
[7]PENG S, LI Z, ZOU L, et al. Improving curcuminsolubility and bioavailability by encapsulation in saponin-coated curcumin nanoparticles prepared using a simple pH-driven loading method [J]. Food & Function. 2018,9(3):1829–1839.
[8]Liu Guoan, Ran Miaomiao, Xu Xinxin, et al. Antioxidant and pro-oxidant - the anti-cancer mechanism of curcumin [J]. Chemistry of Life, 2019, 39 (3): 472-477.
[9]GHORBANZADE T, JAFARI S M, AKHAVAN S, et al. Nano- encapsulation of fish oil in nano-liposomes and its application in fortification of yogurt[J]. Food Chemistry, 2017, 216:146-152.
[10]AKHAVAN S, ASSADPOUR E, KATOUZIAN I , et al. Lipid nano scale cargos for the protection and delivery of food bioactive ingredients and nutraceuticals[J]. Trends in Food Science & Technology, 2018, 74:132-146.
[11]ZHANG W,MAW,ZHANG J, et al. The immunoregulatory activities of astragalus polysaccharide liposome on macrophages and dendritic cells[J]. International Journal of Biological Macromolecules. 2017, 105: 852–861.
[12]SHITYAKOV S, SALMAS R E, DURDAGI S, et al. Solubility profiles, hydration and desolvation of curcumin complexed with γ-cyclodextrin and hydroxypropyl-γ-cyclodextrin[J]. Journal of Molecular Structure, 2017, 1134:91-98.
[13]HE C,ZHANG X,YAN R, et al. Enhancement of cisplatin efficacy by lipid-CaO2 nanocarrier-mediated comprehensive modulation of the tumor microenvironment[J]. Biomaterials Science,2019,7(10):4260-4272.
[14]CHEN X , ZOU L Q, NIU J , et al. The stability, sustained release and cellular antioxidant activity of curcumin nanoliposomes[J]. Molecules, 2015, 20(8):14293-14311.
[15]MEHNERT W , MDER K . Solid lipid nanoparticles: production, characterization and applications[J]. Advanced Drug Delivery Reviews, 2001, 47(2-3):165-196.
[16]EKAMBARAM P, SATHALI A A H, PRIYANKA K. Solid lipid nanoparticles: a review[J]. Scientific Reviews & Chemical Communications. 2012,2(1): 80-102.
[17]NUNES S , MADUREIRA R ,CAMPOS D , et al. Solid lipid nanoparticles as oral delivery systems of phenolic compounds: overcoming pharmacokinetic limitations for nutraceutical applications[J].Critical Reviews in Food Science and Nutrition, 2015,57(9):1863-1873.
[18]KAKKARV , SINGH S , SINGLAD , et al. Exploring solid lipid nanoparticles to enhance the oral bioavailability of curcumin[J]. Molecular Nutrition & Food Research, 2011, 55(3):495-503.
[19 ]RAHMAN M H , RAMANATHAN M,SANKAR V .Preparation, characterization and in vitro cytotoxicity assay of curcumin loaded solid lipid nanoparticle in IMR32 neuroblastoma cell line[J]. Pakistan Journal of Pharmaceutical Sciences, 2014, 27(5):1281-1285.
[20]ABOLFAZL S , AMIRHOSSEIN S . Nanotechnology: a successful approach to improve oral bioavailability of phytochemicals[J]. Recent Patents on Drug Delivery & Formulation, 2016, 10(1):4-6.
[21]WU W, CHEN M, LUO T R, et al. ROS and GSH-responsive S-nitrosoglutathione functionalized polymeric nanoparticles to overcome multidrug resistance in cancer[J]. Acta Biomaterialia. 2020,103:259-271.
[22]EI-SAY K M, EL-SAWY H S. Polymeric nanoparticles: promising platform for drug delivery[J]. International Journal of Pharmaceutics. 2017,528(1-2):675-691.
[23 ]KUMARI P , GHOSH B , BISWAS S . Nanocarriers for cancer-targeted drug delivery[J]. Journal of Drug Targeting, 2016,24(3):179-191.
[24]TSAI Y M , CHIEN C F , LIN L C , et al. Curcumin and its nano-formulation: the kinetics of tissue distribution and blood-brain barrier penetration[J]. International journal of pharmaceutics, 2011, 416(1):331-338.
[25]CHEN Y , LU Y , LEE R J , et al. Nano Encapsulated Curcumin: And Its Potential for Biomedical Applications[J]. International Journal of Nanomedicine, 2020, 15:3099-3120.
[26]WEI X , SENANAYAKE T H , BOHLING A , et al. Targeted nanogel conjugate for improved stability and cellular permeability of curcumin: synthesis, pharmacokinetics, and tumor growth inhibition[J]. Molecular Pharmaceutics, 2014, 11(9):3112-3122.
[27]AHMAD M Z , ALKAHTANI S A , AKHTER S , et al. Progress in nanotechnology-based drug carrier in designing of curcumin nanomedicines for cancer therapy: current state of the art[J]. Journal of Drug Targeting, 2016, 24(4):273-293.
[28] Jiang Xiaohong, Huang Xuan, Huang Xiong, et al. Application of drug-loaded systems-polymer micelles [J]. Chinese Journal of Experimental Pharmacology, 2010, 16(10):220-223.
[29] ABIEE N , DELJOO S , RABIEE M . Curcumin-hybrid nanoparticles in drug delivery system[J]. Asian Journal of Nanosciences and Materials.2018,2(1):66-91.
[30] Chen F, Yang Y, Zhang L, et al. Research progress of curcumin nanomedicines in tumor therapy [J]. Chinese Journal of Modern Applied Pharmacy, 2019, 36(21):2731-2737.
[31] NAKSURIYA O , OKONOGI S , SCHIFFELERS R M , et al. Curcumin nanoformulations: a review of pharmaceutical properties and preclinical studies and clinical data related to cancer treatment[J]. Biomaterials, 2014, 35(10): 3365-3383.
[32 ]BAEK J S, CHO C W. Surface modification of solid lipid nanoparticles for oral delivery of curcumin: Improvement of bioavailability through enhanced cellular uptake, and lymphatic uptake[J]. European Journal of Pharmaceutics & Biopharmaceutics, 2017,117, 132-140.
[33 ]GONG C Y , DENG S Y , WU Q , et al. Improving antiangiogenesis and anti-tumor activity of curcumin by biodegradable polymeric micelles[J]. Biomaterials, 2013, 34(4):1413-1432.
[34]DAVIS B M , PAHLITZSCH M , GUO L , et al. Topical curcumin nanocarriers are neuroprotective in eye disease[J]. Scientific Reports, 2018, 8(1):11066.
[35]LI M S , XIN M , GUO C L , et al. New nanomicelle curcumin formulation for ocular delivery: improved stability, solubility, and ocular anti-inflammatory treatment[J]. Drug Development & Industrial Pharmacy, 2017,43(11):1846-1857.
[36]XIE M B , FAN D J , ZHENG Z , et al. Nano-curcumin prepared via supercritical: Improved anti-bacterial, anti-oxidant and anti-cancer efficacy[J]. International Journal of Pharmaceutics, 2015, 496(2):732-740.
[37]VIMALAK , MOHANY M , SIVUDU K S , et al. Fabrication of porous chitosan films impregnated with silver nanoparticles: a facile approach for superior antibacterial application[J]. Colloids & Surfaces B Biointerfaces, 2010, 76(1):248-258.
[38]MATHEW D , HSU W L . Antiviral potential of curcumin[J]. Journal of Functional Foods, 2018, 40:692-699.
[39]GANDAPU U , CHAITANYA R K , KISHORE G , et al. Curcumin-loaded apotransferrin nanoparticles provide efficient cellular uptake and effectively inhibit HIV-1 replication in vitro[J]. Plos One, 2011, 6(8):1-11.
[40]YANG X X , LI C M , HUANG C Z . Curcumin modified silver nanoparticles for highly efficient inhibition of respiratory syncytial virus infection[J]. Nanoscale, 2016, 8(5):3040-3048.
[41]AKBIK D , GHADIRI M , CHRZANOWSKI W , et al. Curcumin as a wound healing agent[J]. Life Sciences, 2014, 116(1):1-7.
[42]ZAHRA R , MOHAMMAD N , MARJAN D, et al. Application of curcumin-loaded nanocarriers for food, drug and cosmetic purposes[J]. Trends in Food Science & Technology, 2019, 88:445-458.
[43]LI X, CHEN S, ZHANG B , et al. In situ injectable nano-composite hydrogel composed of curcumin, N,O-carboxymethyl chitosan and oxidized alginate for wound healing application[J]. International Journal of Pharmaceutics, 2012, 437(1-2):110-119.


 English
English French
French Spanish
Spanish Russian
Russian Korean
Korean Japanese
Japanese